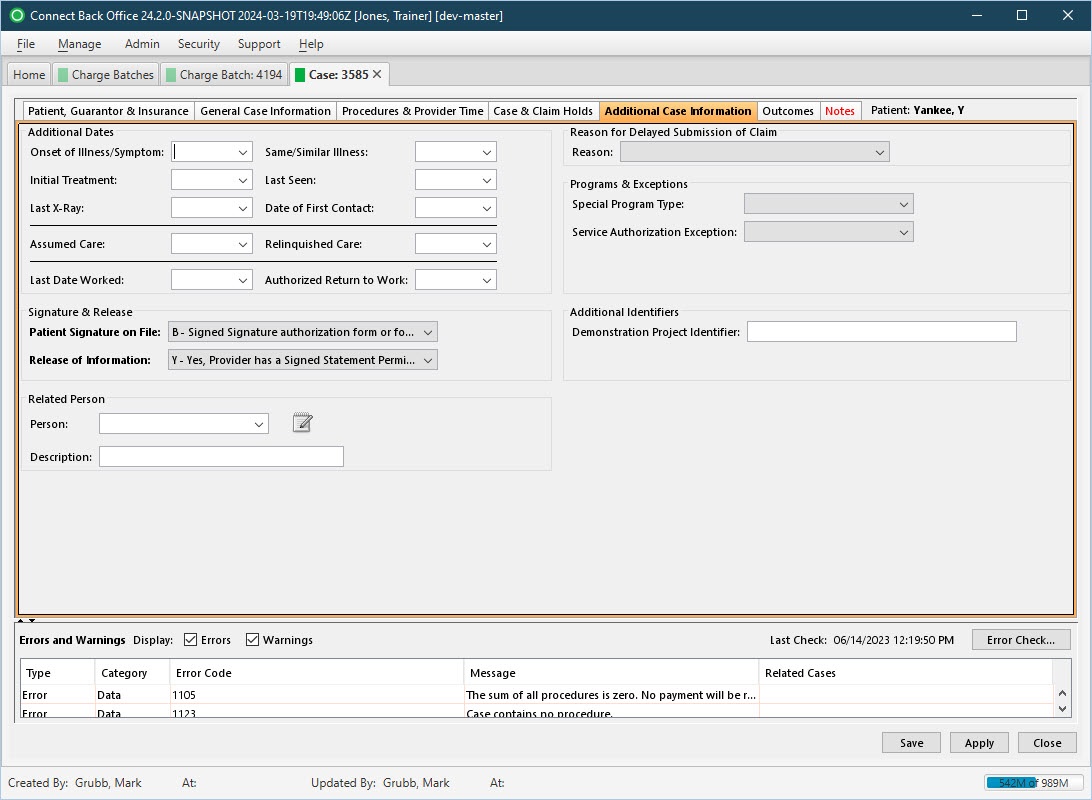
Overview
The Additional Case Information tab collects any additional information about the case, including:
- Additional Dates
- Reason for Delayed Submission of Claim
- Programs & Exceptions
- Signature & Release
Field Definitions
Field | Type | Required | Description | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Additional Dates Section | |||||||||||||||
| Onset of Illness/Symptom | Calendar Date (mm/dd/yyyy) | No | The date the illness or symptom began. | ||||||||||||
| Same/Similar Illness | Calendar Date (mm/dd/yyyy) | No | The date the patient was treated for the same or similar illness. | ||||||||||||
| Initial Treatment | Calendar Date (mm/dd/yyyy) | No | The date the patient was initially treated for the illness or symptom. | ||||||||||||
| Last Seen | Calendar Date (mm/dd/yyyy) | No | The date the patient was last seen by the provider. | ||||||||||||
| Last X-Ray | Calendar Date (mm/dd/yyyy) | No | The date the patient had the last x-ray. | ||||||||||||
| Date of First Contact | Calendar Date (mm/dd/yyyy) | No | The date the provider initially examined the patient. | ||||||||||||
| Assumed Care | Calendar Date (mm/dd/yyyy) | No | The date the provider began caring for the patient. | ||||||||||||
| Relinquished Care | Calendar Date (mm/dd/yyyy) | No | The date the provider no longer provided care for the patient. | ||||||||||||
| Last Date Worked | Calendar Date (mm/dd/yyyy) | No | The date the patient last worked. | ||||||||||||
| Authorized Return to Work | Calendar Date (mm/dd/yyyy) | No | The date the patient is authorized to return to work. | ||||||||||||
| Reason for Delayed Submission of Claim Section | |||||||||||||||
| Reason | Drop Down | No | Indicates why claims have not been submitted, or why submission has been delayed. If the claim is being submitted more than six months after the original date of service, you can specify a reason code indicating the reason for the delay in filing. Options include: 1 - Proof of Eligibility Unknown or Unavailable 2 - Litigation 3 - Authorization Delays 4 - Delay in Certifying Provider 5 - Delay in Supplying Billing Forms 6 - Delay in Delivery of Custom-Made Appliances 7 - Third Party Processing Delay 8 - Delay in Eligibility Determination 9 - Original Claim Rejected or Denied Due to Reason Unrelated to Billing Limitation Rules 10 - Administration Delay in the Prior Approval Process 11 - Other 15 - Natural Disaster | ||||||||||||
| Programs & Exceptions Section | |||||||||||||||
| Special Program Type | Drop Down | No | Indicates the type of special program under which the patient was treated. Options include:
| ||||||||||||
| Service Authorization Exception | Drop Down | No | Indicates the HIPAA recognized exception under which the patient was treated. Options include:
| ||||||||||||
| Signature & Release Section | |||||||||||||||
| Patient Signature on File | Drop Down | Yes | Indicates which form the patient signed to grant authorization for filing the claim on behalf of the patient. By default, this option is set to B - Signed Signature Authorization Form or Forms for Both HCFA-1500 Claim Form Block 12 and Block 13 are on file. This information prints in box 13 on the CMS-1500 claim form. Options include:
| ||||||||||||
| Release of Information | Drop Down | Yes | Indicates whether the provider has authorization from the patient or guarantor to release medical information about the patient. By default, this option is set to Y - Yes, Provider Has a Signed Statement Permitting Release of Medical Billing Data Related to a Claim. This information prints in box 12 on the CMS-1500 claim form. Options include:
| ||||||||||||
| Additional Identifiers Section | |||||||||||||||
| Demonstration Project Identifier | Free Text | No | Records the Demonstration Project Identifier or clinical trial number on a case (up to 50 characters). A Medicare Demonstration Project attempts to gauge the effect of possible changes to the Medicare program. Medicare requires this information when the case includes a Demonstration Project Number. If this data is present on a case, the EDI file will include it in the 2300 loop, REF02 segment with an REF01 P4 qualifier. | ||||||||||||
| Related Person Section | Section allows you to designate a person who is related to the patient. | ||||||||||||||
| Person | Drop Down Search | No | The last and first names of the person related to the patient. | ||||||||||||
| Description | Free Text | No | The relationship of the patient to the related person, for example, spouse, mother, or father. | ||||||||||||
| Errors and Warning Section | This section reports problems detected through the Error Check validation process. Use the Display options to select the validations to verify. In addition to errors and warnings, the date and time the last error check occurred is reported. If an error check has never been performed on a charge batch or case, the text displayed will be Last Check: (pending). Each time an error check is completed, this text is updated and displayed in the following format: Last Check: mm/dd/yyyy, hh:mm:ss AM/PM, for example, Last Check: 07/08/2013, 4:35:14 PM. | ||||||||||||||
| Display Filters | Checkboxes | No | This filter determines the type of errors or warnings listed in the Error Check list. Errors must be corrected before a case or charge batch can be submitted and claims can be generated. Warnings may or may not cause rejection of a claim and are not required to be corrected. A checkmark next to the display filter indicates that the filter is selected. The filter options dynamically affect the contents of the error checklist. When you clear a checkbox, the list hides the applicable errors or warnings. When you click the checkbox again, the list refreshes, showing the hidden errors or warnings. | ||||||||||||
| Type | Read-only (system-generated) | Yes | The classification of the problem detected in a category during the Error Checking process. Cases in the charge batch are validated for certain conditions reported as errors or warnings.
| ||||||||||||
| Category | Read-only (system-generated) | Yes | The component that may contain an error or warning when either condition is detected during error check validation, for example, Concurrency or Data. By default, all categories are selected and all errors and warnings are displayed on the Charge Batch Error Check tab. Errors must be corrected before a claim can be created. Warnings do not have to be corrected before a claim can be created. The categories listed in the error check table are controlled by the Display filters on the Charge Batch Error Check tab. The following categories are available:
| ||||||||||||
| Message | Read-only (system-generated) | Yes | The description of the error or warning. | ||||||||||||
| Related Cases | Link | No | A direct link to cases related to the case that has a warning or error. To go to a related case, click the direct link. If the related case has a warning or error that is corrected, the Error Check validation process will verify the case and remove it from the Charge Batch Error Check tab. |
Button Descriptions
Button | Shortcut Keys | Description | Step-By-Step Guides |
|---|---|---|---|
| Error and Warnings Section | |||
| Error Check | [Alt] + [K] | To run the Error Check validation for either a charge batch or a case in a charge batch. | Running Error Check Validation |
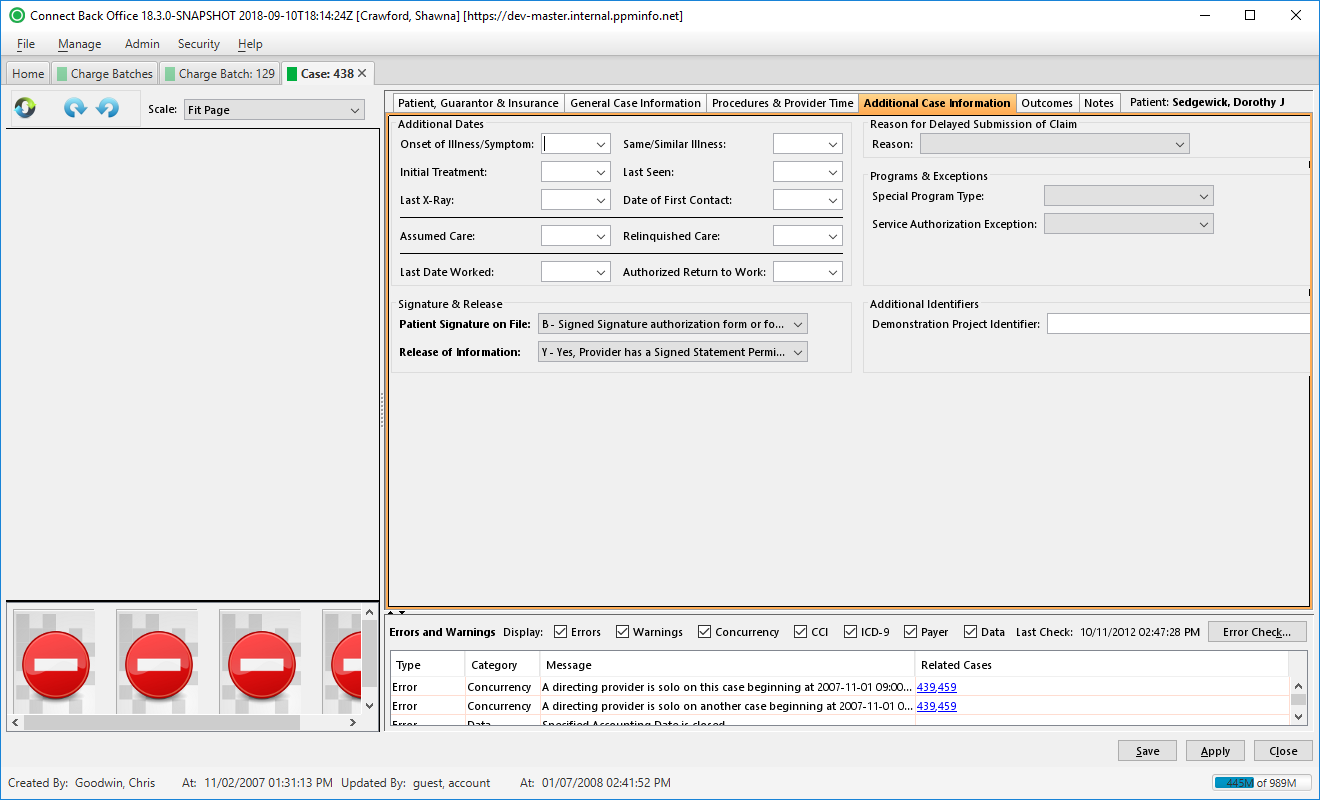
Overview
The Additional Case Information tab collects any additional information about the case, including:
- Additional Dates
- Reason for Delayed Submission of Claim
- Programs & Exceptions
- Signature & Release
Field Definitions
Field | Type | Required | Description | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Additional Dates Section | |||||||||||||||
| Onset of Illness/Symptom | Calendar Date (mm/dd/yyyy) | No | The date the illness or symptom began. | ||||||||||||
| Same/Similar Illness | Calendar Date (mm/dd/yyyy) | No | The date the patient was treated for the same or similar illness. | ||||||||||||
| Initial Treatment | Calendar Date (mm/dd/yyyy) | No | The date the patient was initially treated for the illness or symptom. | ||||||||||||
| Last Seen | Calendar Date (mm/dd/yyyy) | No | The date the patient was last seen by the provider. | ||||||||||||
| Last X-Ray | Calendar Date (mm/dd/yyyy) | No | The date the patient had the last x-ray. | ||||||||||||
| Date of First Contact | Calendar Date (mm/dd/yyyy) | No | The date the provider initially examined the patient. | ||||||||||||
| Assumed Care | Calendar Date (mm/dd/yyyy) | No | The date the provider began caring for the patient. | ||||||||||||
| Relinquished Care | Calendar Date (mm/dd/yyyy) | No | The date the provider no longer provided care for the patient. | ||||||||||||
| Last Date Worked | Calendar Date (mm/dd/yyyy) | No | The date the patient last worked. | ||||||||||||
| Authorized Return to Work | Calendar Date (mm/dd/yyyy) | No | The date the patient is authorized to return to work. | ||||||||||||
| Reason for Delayed Submission of Claim Section | |||||||||||||||
| Reason | Drop Down | No | Indicates why claims have not been submitted, or why submission has been delayed. If the claim is being submitted more than six months after the original date of service, you can specify a reason code indicating the reason for the delay in filing. Options include: 1 - Proof of Eligibility Unknown or Unavailable 2 - Litigation 3 - Authorization Delays 4 - Delay in Certifying Provider 5 - Delay in Supplying Billing Forms 6 - Delay in Delivery of Custom-Made Appliances 7 - Third Party Processing Delay 8 - Delay in Eligibility Determination 9 - Original Claim Rejected or Denied Due to Reason Unrelated to Billing Limitation Rules 10 - Administration Delay in the Prior Approval Process 11 - Other 15 - Natural Disaster | ||||||||||||
| Programs & Exceptions Section | |||||||||||||||
| Special Program Type | Drop Down | No | Indicates the type of special program under which the patient was treated. Options include:
| ||||||||||||
| Service Authorization Exception | Drop Down | No | Indicates the HIPAA recognized exception under which the patient was treated. Options include:
| ||||||||||||
| Signature & Release Section | |||||||||||||||
| Patient Signature on File | Drop Down | Yes | Indicates which form the patient signed to grant authorization for filing the claim on behalf of the patient. By default, this option is set to B - Signed Signature Authorization Form or Forms for Both HCFA-1500 Claim Form Block 12 and Block 13 are on file. This information prints in box 13 on the CMS-1500 claim form. Options include:
| ||||||||||||
| Release of Information | Drop Down | Yes | Indicates whether the provider has authorization from the patient or guarantor to release medical information about the patient. By default, this option is set to Y - Yes, Provider Has a Signed Statement Permitting Release of Medical Billing Data Related to a Claim. This information prints in box 12 on the CMS-1500 claim form. Options include:
| ||||||||||||
| Additional Identifiers Section | |||||||||||||||
| Demonstration Project Identifier | Free Text | No | Records the Demonstration Project Identifier or clinical trial number on a case (up to 50 characters). A Medicare Demonstration Project attempts to gauge the effect of possible changes to the Medicare program. Medicare requires this information when the case includes a Demonstration Project Number. If this data is present on a case, the EDI file will include it in the 2300 loop, REF02 segment with an REF01 P4 qualifier. | ||||||||||||
| Errors and Warning Section | This section reports problems detected through the Error Check validation process. Use the Display options to select the validations to verify. In addition to errors and warnings, the date and time the last error check occurred is reported. If an error check has never been performed on a charge batch or case, the text displayed will be Last Check: (pending). Each time an error check is completed, this text is updated and displayed in the following format: Last Check: mm/dd/yyyy, hh:mm:ss AM/PM, for example, Last Check: 07/08/2013, 4:35:14 PM. | ||||||||||||||
| Display Filters | Checkboxes | No | This filter determines the type of errors or warnings listed in the Error Check list. Errors must be corrected before a case or charge batch can be submitted and claims can be generated. Warnings may or may not cause rejection of a claim and are not required to be corrected. A checkmark next to the display filter indicates that the filter is selected. The filter options dynamically affect the contents of the error checklist. When you clear a checkbox, the list hides the applicable errors or warnings. When you click the checkbox again, the list refreshes, showing the hidden errors or warnings. | ||||||||||||
| Type | Read-only (system-generated) | Yes | The classification of the problem detected in a category during the Error Checking process. Cases in the charge batch are validated for certain conditions reported as errors or warnings.
| ||||||||||||
| Category | Read-only (system-generated) | Yes | The component that may contain an error or warning when either condition is detected during error check validation, for example, Concurrency or Data. By default, all categories are selected and all errors and warnings are displayed on the Charge Batch Error Check tab. Errors must be corrected before a claim can be created. Warnings do not have to be corrected before a claim can be created. The categories listed in the error check table are controlled by the Display filters on the Charge Batch Error Check tab. The following categories are available:
| ||||||||||||
| Message | Read-only (system-generated) | Yes | The description of the error or warning. | ||||||||||||
| Related Cases | Link | No | A direct link to cases related to the case that has a warning or error. To go to a related case, click the direct link. If the related case has a warning or error that is corrected, the Error Check validation process will verify the case and remove it from the Charge Batch Error Check tab. |
Button Descriptions
Button | Shortcut Keys | Description | Step-By-Step Guides |
|---|---|---|---|
| Error and Warnings Section | |||
| Error Check | [Alt] + [K] | To run the Error Check validation for either a charge batch or a case in a charge batch. | Running Error Check Validation |