Overview
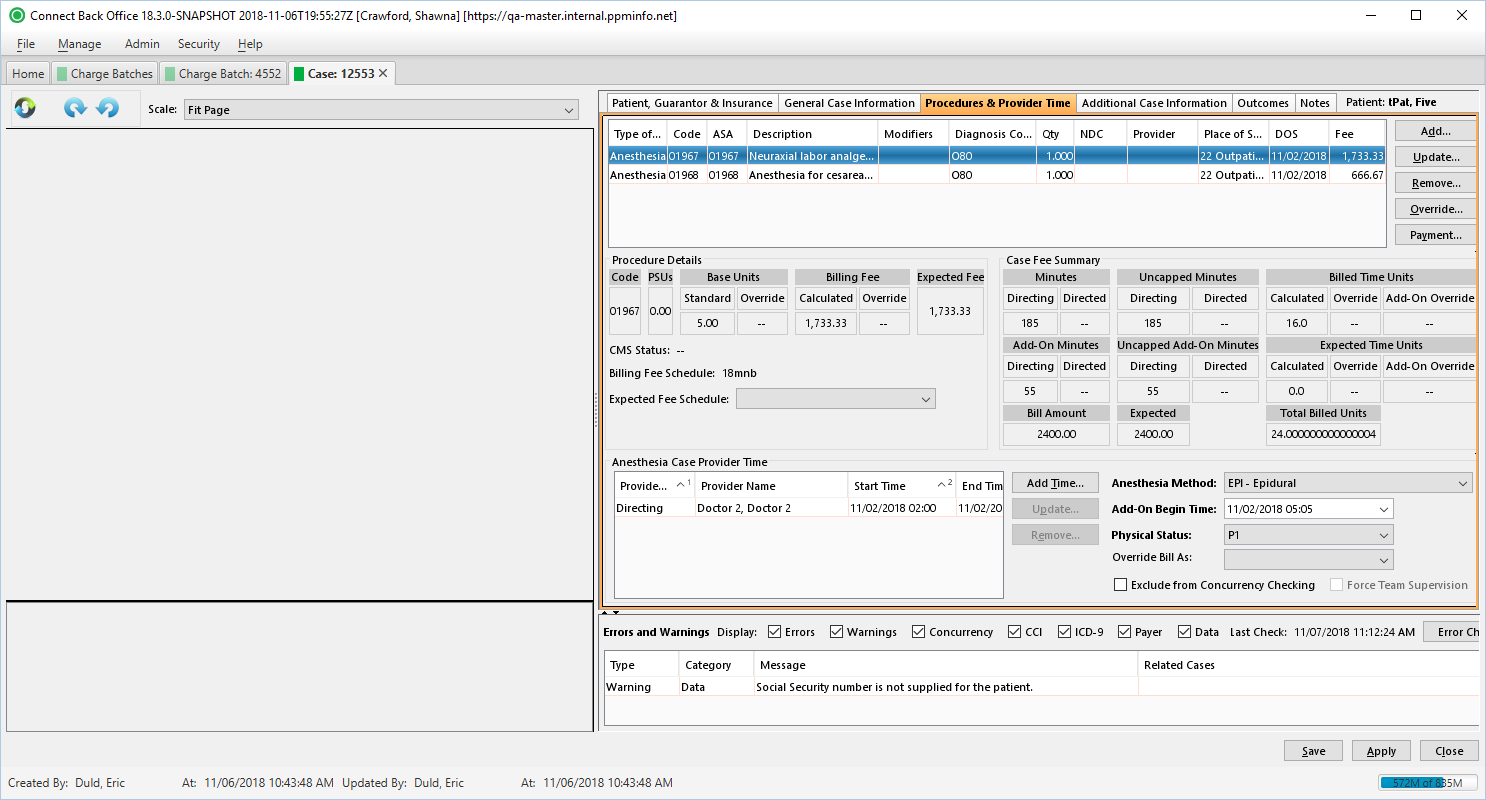
The Procedures & Provider Time tab collects the detailed information of the procedure and provider time related to anesthesia procedures.
Field Definitions
Field | Type | Required | Description | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Procedure Table | The table contains a list of all procedures added to the case. | ||||||||||||||||
| Type of Serv | Display Only (Pulled from added/updated Procedure) | Yes | The type of service provided. When the CPT code is any of the following, this value will be as indicated:
| ||||||||||||||
| Code | Display Only (Pulled from added/updated Procedure) | Yes | The procedure that was performed on the case. If the procedure can be mapped to an anesthesia code, the ASA column contains that anesthesia code. If procedure in the Code column is an anesthesia procedure, the ASA column contains that procedure code. | ||||||||||||||
| ASA | Display Only (Pulled from added/updated Procedure) | No | The corresponding anesthesia code of the procedure.
| ||||||||||||||
| Description | Read-only | Yes | The description of the procedure. This column contains information only and is updated when a procedure is selected in the Code column. | ||||||||||||||
| Modifiers | Display Only (Pulled from added/updated Procedure) | No | The two-character code used to describe the services associated with a procedure. A procedure can have up to four modifiers. | ||||||||||||||
| Diagnosis Codes | Display Only (Pulled from added/updated Procedure) | Yes | The diagnosis codes of the procedure. Each diagnosis code is represented in the priority of the relating diagnosis codes for the procedure. Diagnosis codes are ranked according to the primary diagnosis (1), secondary diagnosis (2), etc. | ||||||||||||||
| Qty | Display Only (Pulled from added/updated Procedure) | Yes | The number of units for the service being rendered, for example, the number of treatments. For an anesthesia procedure, this value is 1. | ||||||||||||||
| NDC | Display Only (Pulled from added/updated Procedure) | No | The National Drug Code of the drug administered by injection, as indicated by the J-Code procedure. | ||||||||||||||
| Provider | Display Only (Pulled from added/updated Procedure) | No | The name of the provider who performed the general procedure on the case. For an anesthesia procedure, this column is blank. Provider ID is required when the case includes a Directed CRNA. | ||||||||||||||
| Place of Serv | Display Only (Pulled from added/updated Procedure) | Yes | The designated place of service for the facility. For claims with Place of Service of 51, 52, 56, or 61:
| ||||||||||||||
| DOS | Display Only (Pulled from added/updated Procedure) | Yes | The date of service for the procedure. For anesthesia procedures, this column will be updated from the provider time after it has been recorded in the Anesthesia Case Provider Time section. The DOS column contains the actual date the service began. For anesthesia procedures that span more than one day, the DOS is calculated based on the date and end time recorded for the provider in Anesthesia Case Provider Time and will be reported in the 837 at the service line level. | ||||||||||||||
| Fee | Read-only (Calculated based on the Billing Fee Schedule) | Yes | The dollar amount for the service fee of the procedure calculated by the billing fee schedule.
When rebilling a service line item without fee changes, you cannot change this value. | ||||||||||||||
| Procedure Details Section | This area provides information about the currently selected procedure in the procedure list. | ||||||||||||||||
| Code | Display Only (pulled from the Billing Fee Schedule) | Yes | The procedure code of the currently selected procedure in the procedure list. | ||||||||||||||
| PSUs | Display Only (pulled from the Billing Fee Schedule) | No | The Physical Status Units (PSUs) for the currently selected anesthesia procedure in the procedure list. If a different physical status modifier is selected on the procedure, this value will be updated, which might cause fees to be recalculated. For a general procedure, dashes will be displayed for this value. | ||||||||||||||
| Base Units | Display Only (pulled from the Billing Fee Schedule) | Yes | The standard base units on the currently selected procedure in the procedure list. If the procedure has an override value on the base unit, that value will also be displayed. Override values will appear in red. Dashes indicate that an override is not present. | ||||||||||||||
| Billing Fee | Read-only (calculated from the Billing Fee Schedule and Anesthesia Provider Time) | Yes | The dollar amount calculated from the billing fee schedule for the currently selected procedure in the procedure list. This value is dynamic and will be updated as changes to the procedures are applied. For example, the Physical Status modifier is changed on an anesthesia procedure. If an override has been applied, the dollar amount of the override will be displayed in red. If an override has not been applied, dashes will be displayed. | ||||||||||||||
| Expected Fee | Read-only (calculated from the Expected Fee Schedule and Anesthesia Provider Time) | Yes | The reimbursement amount expected from the payer or plan for the currently selected procedure in the procedure list. | ||||||||||||||
| CMS Status | Read-only (pulled from CMS) | No | The value assigned by CMS for the currently selected procedure code. The values that can be displayed include:
| ||||||||||||||
| Billing Fee Schedule | Drop Down | Yes | The current billing fee schedule used for calculating procedure fees. The field is a drop down which allows users to override the default fee schedule, as necessary. Fee schedules available from the drop down are only those that are active and affiliated with the current practice. | ||||||||||||||
| Expected Fee Schedule | Display Only (pulled from the Insurance assigned to case) | Drop Down | The expected fee schedule used for calculating the expected fee amount. The default fee schedule can be overridden by selecting another fee schedule from the drop down list. | ||||||||||||||
| Case Fee Summary Section | This area provides information about the provider time on the anesthesia procedure. The information is updated as the provider time is completed. | ||||||||||||||||
| Minutes | Read-only (calculated from the Anesthesia Provider Time) | No | A breakdown of the total minutes tied to the procedure split between Directing and Directed. The maximum number of minutes allowed for the procedure is defined in the fee schedule. | ||||||||||||||
| Uncapped Minutes | Read-only (calculated from the Anesthesia Provider Time) | No | The Uncapped Minutes fields are populated with the true minutes required for the procedure, including those minutes above the capped amount, as defined in the fee schedule. | ||||||||||||||
| Billed Time Units | Read-only (calculated from the Anesthesia Provider Time) | Yes | The billed units for all procedures on the case split between Calculated, Override, and Add-On Override units. | ||||||||||||||
| Add-On Minutes | Read-only (calculated from the Anesthesia Provider Time) | No | A breakdown of the total minutes tied to an ancillary procedure split between Directing and Directed. | ||||||||||||||
| Uncapped Add-On Minutes | Read-only (calculated from the Anesthesia Provider Time) | No | The Uncapped Add-On Minutes fields are populated with the true minutes required for an ancillary procedure, including those minutes above the capped amount, as defined in the fee schedule. | ||||||||||||||
| Expected Time Units | Read-only (calculated from the Anesthesia Provider Time) | Yes | The units expected to be paid for all procedures on the case split between Calculated, Override, and Add-On Override units. | ||||||||||||||
| Bill Amount | Read-only (calculated from the Billing Fee Schedule and Anesthesia Provider Time) | Yes | The amount that was billed for total charges for each procedure. It should match the Billing Fee. | ||||||||||||||
| Expected | Read-only (calculated from the Expected Fee Schedule and Anesthesia Provider Time) | No | The expected amount of payment from the responsible party for the amount billed, which is determined by the expected fee schedule configured at the practice configuration. | ||||||||||||||
| Total Billed Units | Read-only (calculated from the Billing Fee Schedule) | Yes | The total of all base + time + physical status units. | ||||||||||||||
| Anesthesia Case Provider Time Section | |||||||||||||||||
| Provider Role | Display Only (pulled from Provider Type field on Add Provider Time window) | Yes | The role the provider performed while administering anesthesia: Directing, Directed, or Observing. | ||||||||||||||
| Provider Name | Display Only (pulled from Provider field on Add Provider Time window) | Yes | The last, first, and title of the provider who performed the anesthesia procedure specified. | ||||||||||||||
| Start Time | Display Only (pulled from Start Time field on Add Provider Time window) | Yes | The date and time the provider started the anesthesia procedure as specified. The provider time can span days within a time range for an individual provider. For example, a procedure started on 09-14-2014 at 19:00 and ended on 09-15-2014 at 00:52 for a solo provider. This time can be entered as one start and end time entry as 09-14-2014 19:00 (start time) and 09-15-2014 00:52 (end time). If the procedure includes an add-on procedure (for example, 01967 and 01968), the time can be entered as a single entry with the start time for the add-on procedure entered in the Add-On Begin Time field. | ||||||||||||||
| End Time | Display Only (pulled from End Time field on Add Provider Time window) | Yes | The date and time the provider ended the anesthesia procedure as specified. The provider time can span days within a time range for an individual provider. For example, a procedure started on 09-14-2014 at 19:00 and ended on 09-15-2014 at 00:52 for a solo provider. This time can be entered as one start and end time entry as 09-14-2014 19:00 (start time) and 09-15-2014 00:52 (end time). If the procedure includes an add-on procedure (for example, 01967 and 01968), the time can be entered as a single entry with the start time for the add-on procedure entered in the Add-On Begin Time field. | ||||||||||||||
| Exclude | Display Only (pulled from checkbox on Add Provider Time window) | No | To exclude the time segment from concurrency checking, the Exclude from Concurrency Checking checkbox is selected in the Add Provider Time window when adding time. If selected, the Exclude column is checked. This differs from the Exclude from Concurrency Checking option to the right of the table, which excludes the entire case from concurrency checking validation. | ||||||||||||||
| Anesthesia Method | Drop Down | Yes | The method used to administer the anesthesia. The options include::
If you change the Physical Status field value, the data displayed in the PSUs column under Procedure Details will be updated, which might cause the fees to be recalculated. When rebilling a service line item without fee changes, you cannot change this value. | ||||||||||||||
| Add-On Begin Time | Calendar Date and Time (mm/dd/yyyy hh:mm) | No | The time at which the transition from a primary procedure to a secondary procedure occurred on the case, if applicable. For example, suppose the primary procedure started as anesthesia for a vaginal delivery, but then evolved into a secondary procedure as anesthesia for a C-section. In this case, you would enter the start time of the secondary procedure, which is the anesthesia related to the C-section. The Add-On Begin Time option is only available when procedures 01968 and 01969 are entered in the procedure details table. The primary procedure and the add-on procedure must be entered in the procedure details table. In addition, both the primary procedure and the add-on procedure must be included in the current billing fee schedule. If either 01968 or 01969 procedure (anesthesia add-on procedure) is included in the procedure details table, the add-on begin time is required. By default, this information is blank. | ||||||||||||||
| Physical Status | Drop Down | Yes | The billing unit value added to an anesthesia procedure to indicate the complexity of the procedure regarding the physical status of the patient. The billing unit values are used to calculate anesthesia fees. The supported physical status modifiers are P1 through P6. This information is required if the procedure is an anesthesia procedure. By default, this option is blank. Select a value from P1 to P6 for the physical condition of the patient. The following table contains the description of each modifier according to the American Society of Anesthesiologists (ASA) ranking of patient physical status:
| ||||||||||||||
| Override Bill As | Drop Down | No | The option for overriding the billing provider to bill as a different provider than the one who performed the anesthesia procedure. For example, the physician instead of the CRNA who actually performed the anesthesia procedure. By default, this information is blank. To bill as a different provider, choose the provider from the list. The provider you choose will be listed on the claim instead of the provider who performed the service. | ||||||||||||||
| Exclude from Concurrency Checking | Checkbox | No | Indicates if the case will not be validated for concurrency exceptions. This option is specific to anesthesia and can only be selected if the procedure includes anesthesia. Use caution when selecting this option as concurrency exceptions will not be reported, which could result in fraudulent billing. By default, this option is blank. To exclude the case from concurrency validation, click the checkbox. If you click this option, the following message appears: Excluding this case from concurrency checking may result in fraudulent billing. Click No to close the message without activating this option. Click Yes to stop concurrency validation on this case. When rebilling a service line item without fee changes, you cannot change this value. | ||||||||||||||
| Force Team Supervision | Checkbox | No | Indicates that not all medical supervision conditions might have been met for medical direction on the case. The case will be billed as medical supervision. At least one Directing provider and one Directed provider must be specified in the Anesthesia Case Provider Time section. Not following the medical direction criteria may result in an audit. By default, this option is blank. Click this option to apply the supervising modifier on the case. If you click this option, the following message appears: Enabling team supervision will cause the case to be billed as medical supervision. This indicates that not all medical supervision conditions have not been met for medical direction. Click No to close the message without activating this option. Click Yes to apply the supervising modifier to this case. When rebilling a service line item without fee changes, you cannot change this value. | ||||||||||||||
| Errors and Warning Section | This section reports problems detected through the Error Check validation process. Use the Display options to select the validations to verify. In addition to errors and warnings, the date and time the last error check occurred is reported. If an error check has never been performed on a charge batch or case, the text displayed will be Last Check: (pending). Each time an error check is completed, this text is updated and displayed in the following format: Last Check: mm/dd/yyyy, hh:mm:ss AM/PM, for example, Last Check: 07/08/2013, 4:35:14 PM. | ||||||||||||||||
| Display Filters | Checkboxes | No | This filter determines the type of errors or warnings listed in the Error Check list. Errors must be corrected before a case or charge batch can be submitted and claims can be generated. Warnings may or may not cause rejection of a claim and are not required to be corrected. A checkmark next to the display filter indicates that the filter is selected. The filter options dynamically affect the contents of the error checklist. When you clear a checkbox, the list hides the applicable errors or warnings. When you click the checkbox again, the list refreshes, showing the hidden errors or warnings. | ||||||||||||||
| Type | Read-only (system-generated) | Yes | The classification of the problem detected in a category during the Error Checking process. Cases in the charge batch are validated for certain conditions reported as errors or warnings.
| ||||||||||||||
| Category | Read-only (system-generated) | Yes | The component that may contain an error or warning when either condition is detected during error check validation, for example, Concurrency or Data. By default, all categories are selected and all errors and warnings are displayed on the Charge Batch Error Check tab. Errors must be corrected before a claim can be created. Warnings do not have to be corrected before a claim can be created. The categories listed in the error check table are controlled by the Display filters on the Charge Batch Error Check tab. The following categories are available:
| ||||||||||||||
| Message | Read-only (system-generated) | Yes | The description of the error or warning. | ||||||||||||||
| Related Cases | Link | No | A direct link to cases related to the case that has a warning or error. To go to a related case, click the direct link. If the related case has a warning or error that is corrected, the Error Check validation process will verify the case and remove it from the Charge Batch Error Check tab. |
Button Descriptions
Button | Shortcut Keys | Description | Step-By-Step Guides |
|---|---|---|---|
| Add | [Alt] + [D] | To add a procedure. | See Steps 43-58 |
| Update | [Alt] + [U] | To modify a procedure. | See Steps 44-59 |
| Remove | [Alt] + [R] | To delete a procedure. |
The procedure is deleted unless one or more of the following conditions apply:
|
| Override | [Alt] + [O] | To apply override values to a procedure. | See Step 44 Additional Information |
| Payment | [Alt] + [Y] | To apply a guarantor payment against a procedure(s) on the case. |
The payments can only be applied from this page to the case prior to it's submission. If the payment has already been created against this case, the Payment button opens the Add Distribution window in read only format to view the payment information. |
| Anesthesia Case Provider Time Section | |||
| Add Time | [Alt] + [T] | To record provider time on an anesthesia procedure. | See Steps 59-70 |
| Update | [Alt] + [P] | To modify provider time. | See Steps 60-71 |
| Remove | [Alt] + [E] | To delete provider time. |
|
| Error and Warnings Section | |||
| Error Check | [Alt] + [K] | To run the Error Check validation for either a charge batch or a case in a charge batch. | Running Error Check Validation |