Overview
- General Tab
- Claims Tab
- Statements Tab
- Anesthesia Tab
- Provider IDs Tab
- Referring Physician IDs Tab
- Facility IDs Tab
- Group IDs Tab
- Practices Tab
- Paper Claim Options Tab
- Electronic Claim Options Tab
- Other Insurance Codes Tab
The Provider IDs tab collects the unique identification numbers issued by the plan to providers. Use the Provider IDs tab to record identification numbers issued by the plan to each provider whether the provider participates with the plan or not. By default, the plan inherits the provider identification numbers recorded in its parent payer configuration.
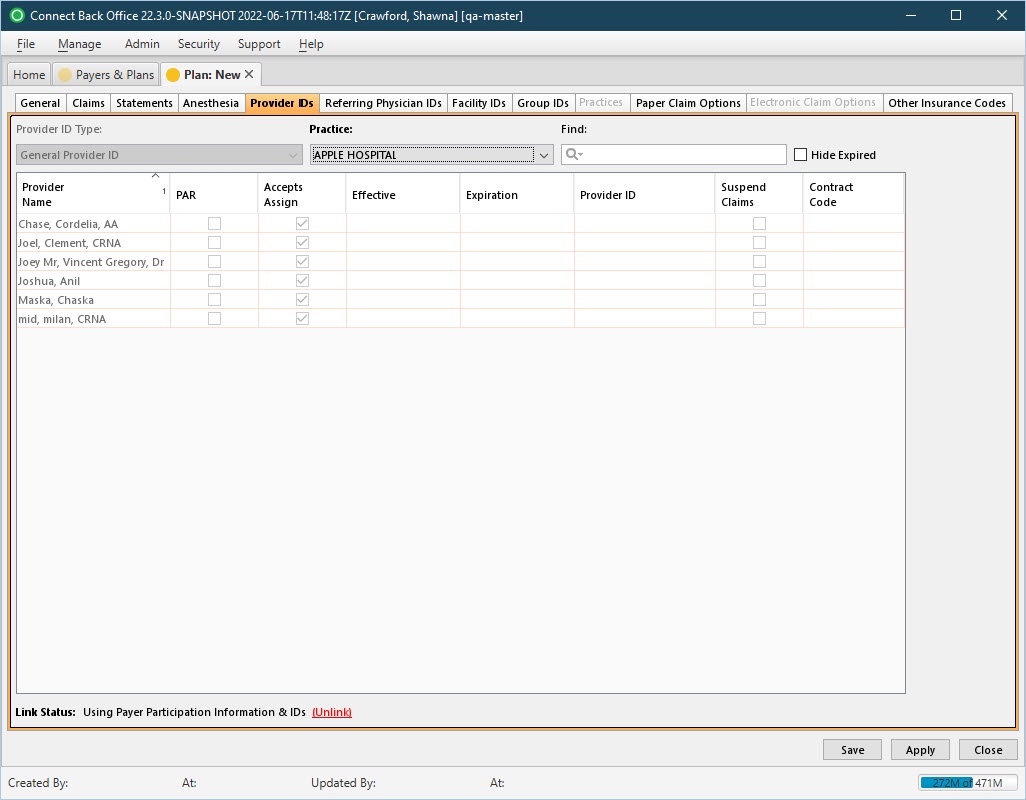
Note: This tab is not accessible from the Plan: New page until the General tab has been populated and applied.
(Click an image below to enlarge.)
Plan: New Page / Provider IDs Tab
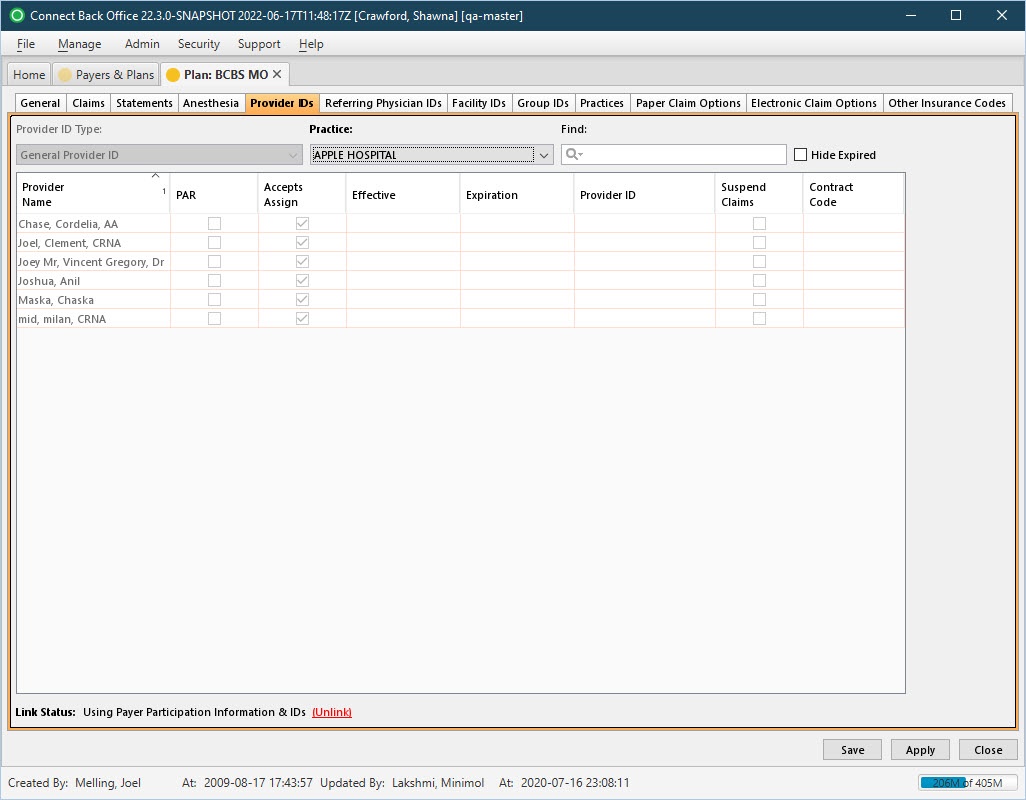
Plan: [name] Page / Provider IDs Tab
Field Definitions
Field | Type | Required | Description |
|---|---|---|---|
| Provider ID Type | Filter | Yes | Specifies whether provider identification numbers are issued for general use or for facility-specific use. Options include:
|
| Practice | Filter | Yes | The list of the practices to which providers are affiliated. |
| Find | Search | No | Filter for locating a provider. The provider name or identification number can be entered. The values entered are matched to the items in the list as you type. |
| Hide Expired | Checkbox | No | If checked, hides the providers who are not currently active. If not checked, both active and inactive providers are displayed. |
| Provider Name | Display Only (Pulled from created/updated Providers) | Yes | The name of the provider. By default, the provider name is listed by last name, first name in ascending order. |
| PAR | Checkbox | No | Indicates whether the provider participates in the payer or plan as a network provider. If checked, the provider is PARticipating. Use the effective and expiration dates to manage the status of PARticipating and non-PARticipating providers.
|
| Accepts Assign | Checkbox | No | Indicates whether the provider can receive reimbursement directly from the payer or plan on behalf of the patient, and that the provider accepts the contractual amount for reimbursement. If PAR is selected, the Accepts Assign option is automatically selected.
If the PAR option is cleared, the Accepts Assign can be selected independently. Select this option if the patient has given the provider permission to accept payment from the payer or plan on the behalf of the patient; otherwise leave blank. |
| Effective | Date (mm/dd/yyyy) | Yes (for PAR provider) | The date the provider begins accepting the insurance of the payer or plan as either a non-PARticipating or a PARticipating provider. For a PAR provider, this date is required. |
| Expiration | Date (mm/dd/yyyy) | No | The date the provider no longer participates in the payer or plan, or the day before a non-PARticipating provider goes to a PARticipating provider. Typically, this date is the expiration date of the payer or plan contract. Use the effective and expiration dates to manage the status of PARticipating and non-PARticipating providers.
For example, the provider starts participating on 03/01/2016. Enter 02/29/2016 as the expiration date in the existing row, then click Add to add a new row. In the new row, select the PAR checkbox, and then enter 03/01/2012 as the effective date, and the provider identification number in the appropriate columns. |
| Provider ID | Free Text | No | The general identification number issued to the provider by the payer or plan. This column appears when the Provider ID Type is set to General Provider ID. |
| Suspend Claims | Checkbox | No | Indicates claims will not be generated for a particular provider. If checked, all claims submitted from a provider are suspended. If charges are entered for the provider in Connect Back Office, an error displays during the error checking process, and no claims are generated for the provider. |
| Contract Code | Free Text | No | Specifies the contract code for the payer or plan. For Medicaid OK, type the applicable contract code in this column to include this code in the 2300 loop, CN1 segment of the electronic claim. |
| Facility Provider IDs | Drop Down / Free Text | No | The facility identification number issued to the provider by the payer or plan. This column appears when the Provider ID Type is set to Facility-Specific. Note: To populate the field, open the drop down list and then enter the Provider ID next to the relevant facility in the list. |
| Link Status | Display Only (Based on Restore Link/Unlink option selected) | Yes | By default, the plan inherits the provider identification numbers recorded in its parent payer configuration. If the plan issues different identification number, the payer and plan identification numbers can be unlinked. The Link Status provides the current status, if the payer and plan IDs are linked or unlinked. |