Overview
The Fee Schedule: New and Fee Schedule: [name] pages are comprised of six tabs:
- General Fee Schedule Information Tab
- Anesthesia Billing Information Tab
- General Procedures Tab
- Anesthesia Procedures Tab
- Miscellaneous Tab
- Audit Tab
The General Fee Schedule Information tab collects general information about the fee schedule and associates payers and plans to the fee schedule.
See the Configuring Fee Schedules topic for additional details.
(Click an image below to enlarge.)
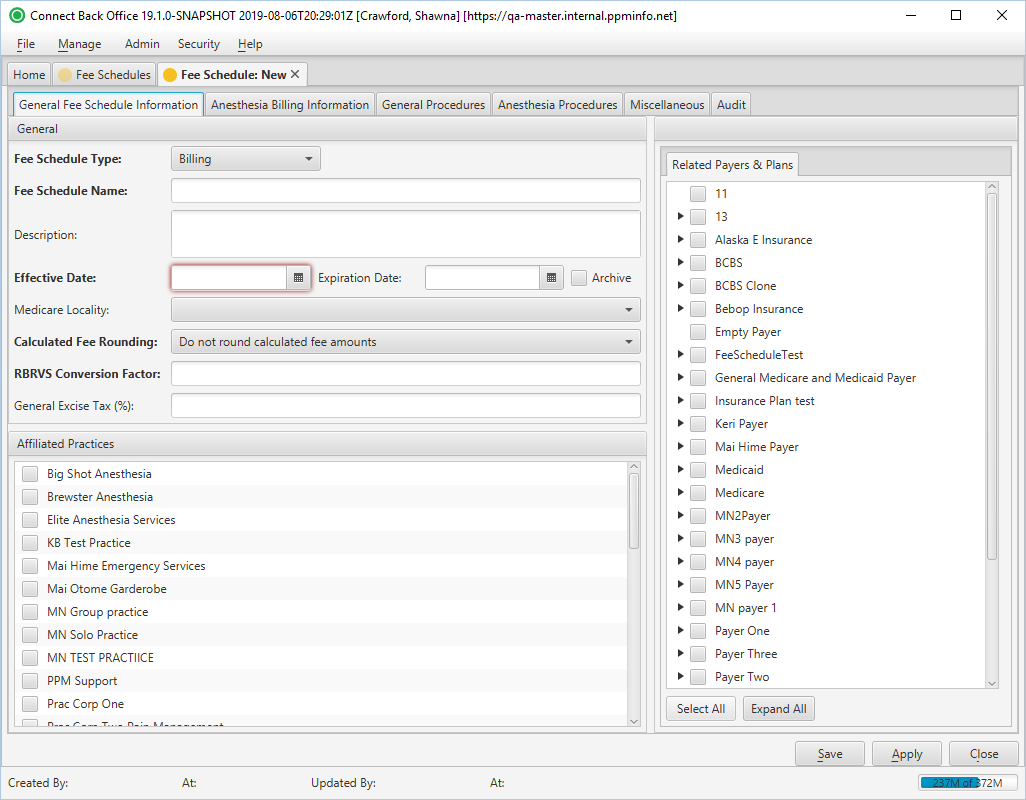
Fee Schedule: New Page / General Fee Schedule Information Tab
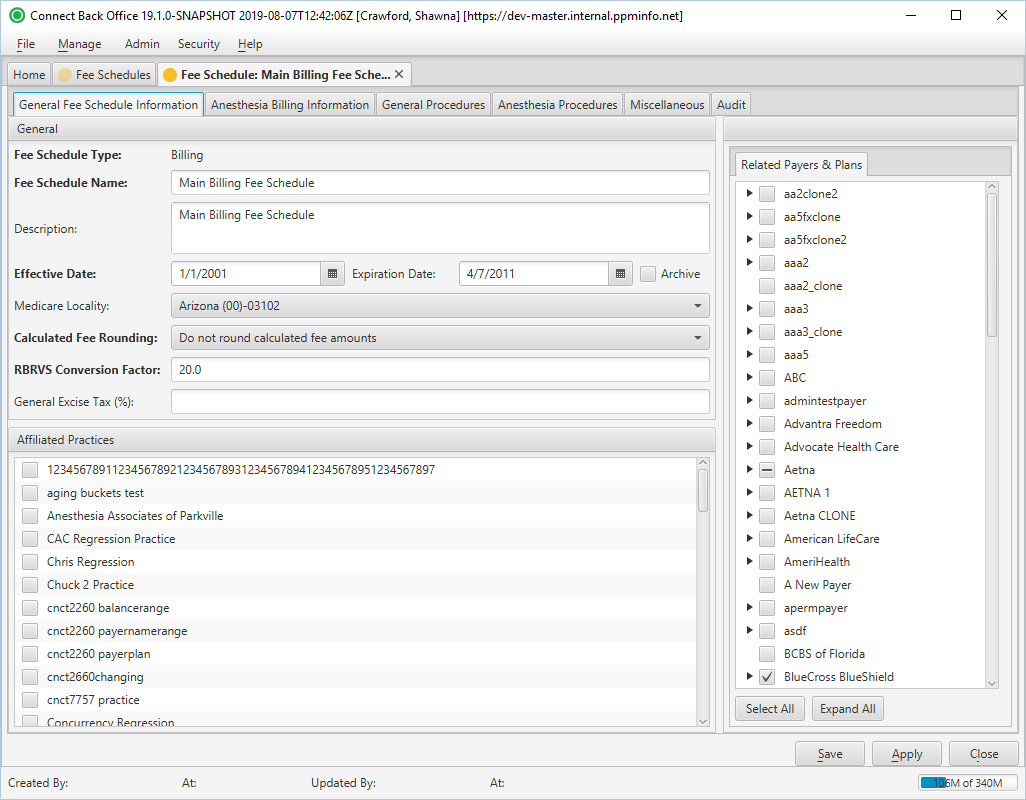
Fee Schedule: [name] Page / General Fee Schedule Information Tab
Field Definitions
Field | Type | Required | Description |
|---|---|---|---|
| General Section | |||
| Fee Schedule Type | Display Only (pulled from created/updated Fee Schedule) | Yes | Identifies if the fee schedule is
|
| Fee Schedule Name | Free Text | Yes | The name of the fee schedule as established in the fee schedule configuration. The name must be unique. To make the fee schedule easy to identify, use the year the fee schedule is effective. Multi-practice groups should include the practice abbreviation in the name to easily identify with which practice it is associated. |
| Description | Free Text | No | The purpose of the fee schedule. Includes any additional information about the fee schedule to make it easy to identify. This field is limited to 1000 characters. |
| Effective Date | Date (mm/dd/yyyy) | Yes | The date the fee schedule starts calculating charges. This date may be prior to the date you begin using the Connect platform. The effective date must be the earliest date which charges will be recorded in Connect Back Office. |
| Expiration Date | Date (mm/dd/yyyy) | No | The date the fee schedule is no longer used to calculate charges. Typically, this date is the expiration date of the payer contract. |
| Archive | Checkbox | No | If checked, the fee schedule is archived and does not display in the list of fee schedules. Archived fee schedules can be accessed by searching for archived items via the Status field in the Search Criteria window. |
| Medicare Locality | Drop Down | No | The Geographic Practice Cost Index (GPCI) used to calculate fees related to charges submitted to Medicare based on geographic location. If left blank, fees are not calculated based on GPCI. If applicable, select the geographical location from the list. The list is maintained from the list provided by CMS. |
| Calculated Fee Rounding | Drop Down | Yes | The method used for rounding the calculated amount for the RBRVS conversion factor. By default, this option is set to Do not round calculated fee amounts. The options include:
|
| RBRVS Conversion Factor | Free Text (Positive, Numeric) | Yes | The flat fee rate of the conversion factor for relative value units. You can enter up to four decimal places, for example, 10.1230. This value will be multiplied by the number of relative value units (RVU) designated in the procedure. For example, suppose the RBRVS conversion factor is 100.00 and the relative value units is 13.6100. The fee for the procedure will be calculated as $1361.00. If the practice does not use 100 to calculate fees for general procedures, you can enter the average conversion factor for the entire practice.
|
| General Excise Tax (%) | Free Text (Numeric) | No | The percentage value used to calculate plans including a general excise tax. |
| Related Payers & Plans Tab | |||
| Related Payers & Plans | Display Only with Selection Checkboxes (Pulled from created/updated Payers & Plans) | Yes | The list of payers and plans in Connect and association checkboxes. Checked payers and plans are linked to the billing fee schedule with fees calculated by the fee schedule. At least one payer and one plan must be selected. A plan can only be assigned to one fee schedule. If the plan is assigned to more than one fee schedule, an error message will display upon trying to save the fee schedule. |
| Special Compensation Days Tab | Tab is only available if the fee schedule type is set to Compensation. | ||
| Name | Display Only (pulled from created/updated Fee Schedule) | No | The name of the special compensation day. |
| Date | Display Only (pulled from created/updated Fee Schedule) | No | The date of the special compensation day. |
| Affiliated Practices Section | |||
| Affiliated Practices | Display Only with Selection Checkboxes (Pulled from created/updated Practices) | Yes | The list of practices in Connect and association checkboxes. A checked box next to a practice indicates the fee schedule is available for use on it. An unchecked box indicates the fee schedule is not available for use on it. |