Overview
| Panel | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||
|
(Click an image below to enlarge.)
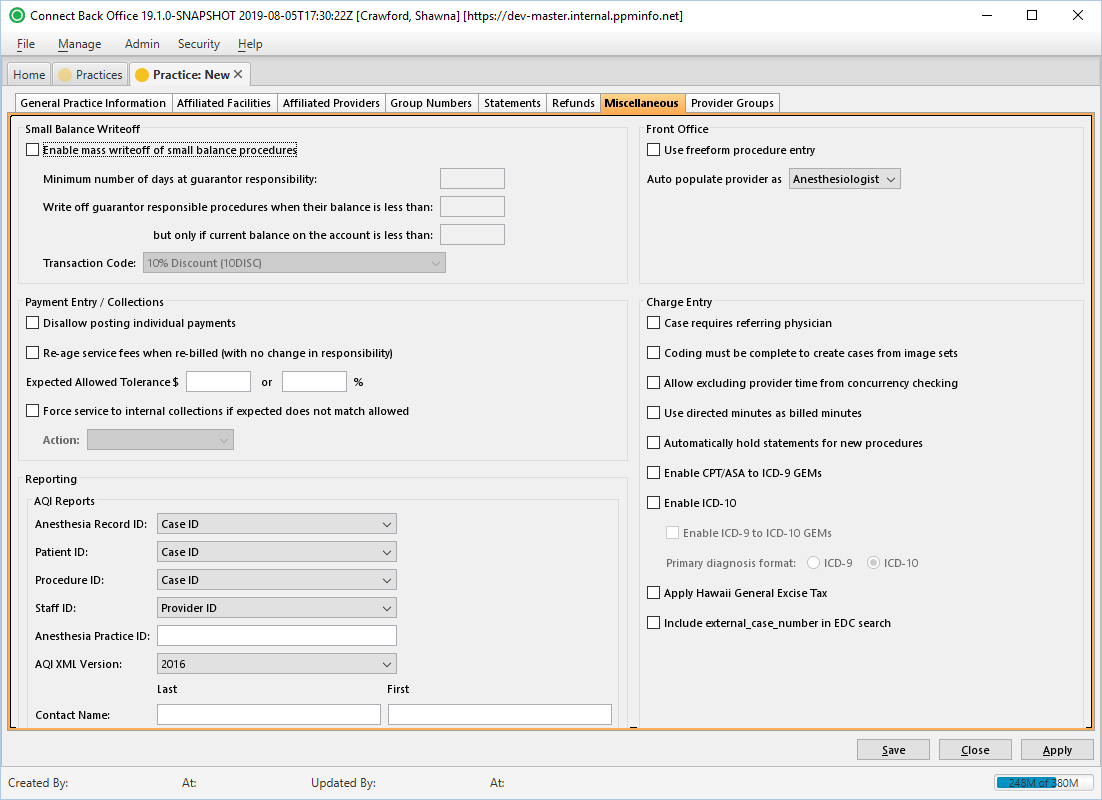
Practice: New Page / Miscellaneous Tab
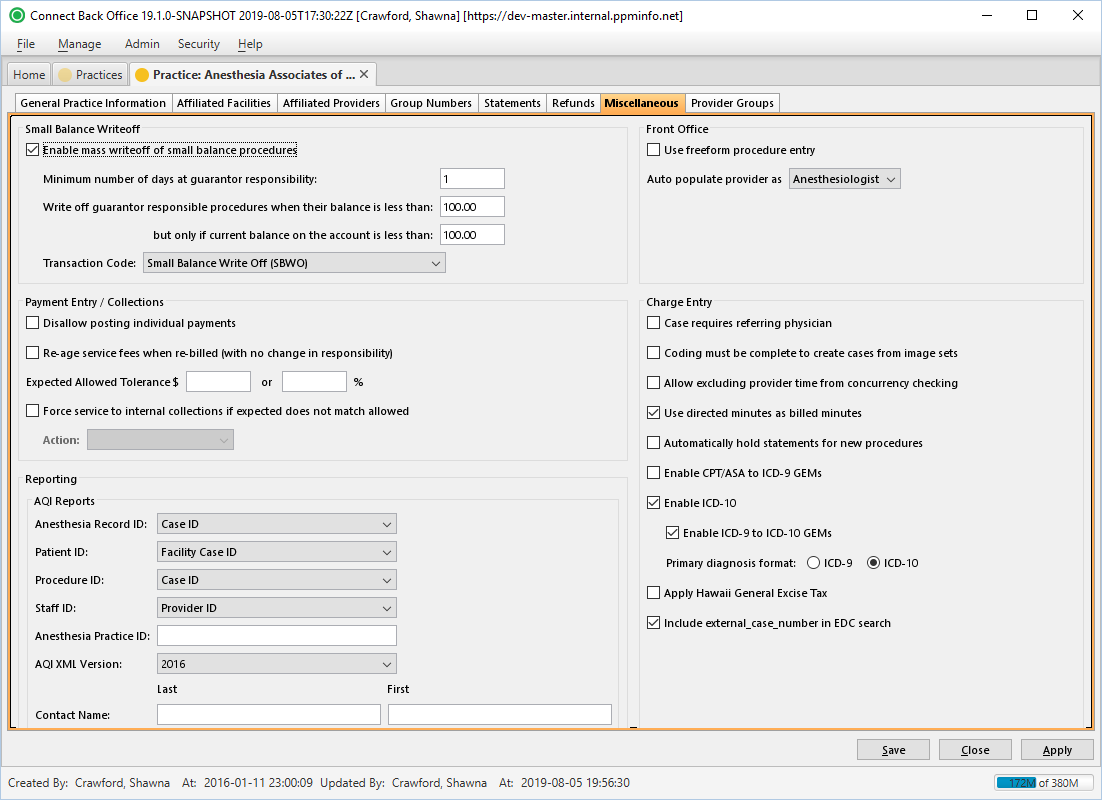
Practice Practice: [name] Page / Miscellaneous Tab
Field Definitions
Field | Type | Required | Description |
| Small Balance Writeoff Section |
| Enable mass writeoff of small balance procedures |
| Checkbox |
| No | Specifies criteria for automatically writing off small balances that originated from a procedure. A small balance must meet all of the following criteria to be eligible for writeoff:
|
|
|
|
|
| Transaction Code | Drop Down | No | Specifies what transaction code the small balance writeoff is posted under. |
Required if Enable mass writeoff of small balance procedures is selected. |
| Payment Entry / Collections Section |
| Require Control Number | Checkbox | No | If selected, requires a control number to be entered when created an insurance payment. If not entered, and the option is selected, a message "Control Number is a required field" will display upon trying to save. |
| Disallow posting individual payments |
| Checkbox |
| No | Prevents the posting of individual payments within a payment batch. When this option is selected, payments may only be posted from the Payment Batches page. This option is available only when the Payment Batch: [ID] > Expected Count and Expected Total values match what was entered during payment entry. |
| Re-age service fees when re-billed (with no change in responsibility) |
| Checkbox |
| No | Resets the responsible balance date to the rebill date, given that responsibility remains the same (guarantor to guarantor, primary to primary, etc.). |
If unchecked, the original bill date is recognized as the responsible balance date. |
Option is checked by default. |
| Expected Allowed Tolerance |
Free Text (Numeric) | No |
Specifies the over-under criteria |
that the Actual Allowed amount from an EOB must |
exceed the Expected Allowed |
amount for inclusion in the Payment Exceptions Report, which is generated from the Payment Batch [ID] page in Back Office. If an Actual Allowed amount from an EOB |
exceeds the set thresholds, the amounts entered in these fields |
determine if the payment is included in the report. You may enter either a dollar amount or a percentage (of the total expected allowed amount). If both values are entered, the inclusion in the report |
is decided based on the lesser amount.
|
|
|
|
|
| |
| Force service to internal collections if expected does not match allowed |
| Checkbox |
| No | Forces service fee lines |
outside of the Expected Allowed Tolerance range to internal insurance collections and the |
assigned Action Type assigned is initiated. Examples:
|
|
|
|
|
| |||
| Action | Drop Down | No | Defines the collection action initiated if the services fee lines are outside the Expected Allowed Tolerance range and sent to internal insurance collections. Only enabled and required if |
Force service to internal collections if expected does not match allowed |
is checked. |
Choosing Anesthesiologist will cause the Anesthesiologist field in the New Provider Appointment window to auto-populate with a list of practice providers and can-schedule providers. The Primary Surgeon field will auto-populate with a list of referring physicians.
Choosing Primary Surgeon will cause the Primary Surgeon field in the New Provider Appointment window to auto-populate with the list of practice providers and can-schedule providers. The Anesthesiologist field will auto-populate with the list of referring physicians.
This option was previously located in Front Office.
Case requires referring physician
| Reporting Section | |||
| AQI Reports Sub-section | Facilitates customization of data sent to AQI. | ||
| Anesthesia Record ID | Drop Down | Yes | The entity selected in the drop down determines the value pulled from the Connect database and reported in the Anesthesia Record ID field of a generated AQI XML file. Options include: Case ID, External Case ID, Facility Case ID, any custom-created fields. |
| Patient ID | Drop Down | Yes | The entity selected in the drop down determines the value pulled from the Connect database and reported in the Patient ID field of a generated AQI XML file. Options include: Case ID, External Case ID, Facility Case ID, any custom-created fields. |
| Procedure ID | Drop Down | Yes | The entity selected in the drop down determines the value pulled from the Connect database and reported in the Procedure ID field of a generated AQI XML file. Options include: Case ID, External Case ID, Facility Case ID, any custom-created fields. |
| Staff ID | Drop Down | Yes | The entity selected in the drop down determines the value pulled from the Connect database and reported in the Staff ID field of a generated AQI XML file. Options include: Provider ID, Tax ID_NPI. |
| Anesthesia Practice ID | Free Text | No | Allows the entry of an alphanumeric value. The value represents the Practice ID for AQI reporting purposes. |
| AQI XML Version | Drop Down | Yes | Used to identify the XML version used by the practice. |
| QI Number (Fides) | Drop Down | Yes | Designates the QI to include with the Fides extract report. |
| Charge Entry Section | |||
Case requires referring physician | Checkbox | No |
Designates the Referring Physician field as required in Back Office. | |
Coding must be complete to create cases from image sets |
| Checkbox |
| No | Blocks the creation of a case from an image set in Back Office before the Coding form is completed in Image Batches of Back Office |
. To restrict cases from being created from image sets before the Coding status is complete, check the box. To allow cases from image sets regardless of the Coding status, leave the |
checkbox blank. |
Allow excluding provider time from concurrency checking |
| Checkbox |
| No | Allows users of Connect Back Office to check the |
Exclude (provider time segment) from concurrency checking option when using the Add/Update Provider Time form in charge entry. Excluded minutes will continue to be considered in total case time and start/stop time. When a time segment is excluded, a pop-up alert appears. |
Use directed minutes as billed minutes |
| Checkbox |
| No | Uses the directed provider's minutes as the billed minutes for the purpose of calculating directed provider billed minutes and time units.
|
|
|
|
|
|
|
|
| |
Automatically hold statements for new procedures |
| Checkbox |
| No |
Hold statements for all new cases and procedures at the practice level. Once this box is checked, Connect Back Office |
automatically |
checks the Hold Statement |
checkbox in charge entry on all new procedures. The charge entry Hold Statement option |
also automatically |
becomes unavailable to the user until the box is unchecked. When held procedures are highlighted in charge entry, an indicator appears in the Procedure Details |
Enable CPT/ASA to ICD-9 GEMs (General Equivalence Mappings)
Populates ICD-9 Code line in Back Office Charge Entry (Add/Update Procedure dialog box) with potential diagnosis code matches based on the CPT code(s) entered. By default, this option is not checked.
Enable ICD-10
Enables the ICD-10 fields and drop downs in Back Office Charge Entry (Add/Update Procedure dialog box). By default, this option is not checked.
Populates mapping options between ICD-9 and ICD-10 diagnosis codes. By default, this option is not checked. This functionality works both ways (ICD-9 to ICD-10 and ICD-10 to ICD-9), depending on the Primary diagnosis format selected (see below). For example, if ICD-9 is selected as the Primary diagnosis format and an ICD-9 Code is selected, the GEM Scenario and Choice Selection dialog box appears and allows the user to choose an ICD-10 code or codes to map to.
If the Enable CPT to ICD-9 GEMs is unchecked and the ICD-9 code entered is not associated with the Procedure (CPT) code, an error will advise the user that the ICD-9 code is not associated with the CPT.
If ICD-10 is set a the Primary diagnosis format, the Enable CPT to ICD-9 GEMs option does not function, regardless of whether it is checked. The system will instead identify only ICD-9 Code crosswalks for the selected ICD-10 Code.
section. | |||
| Diagnosis Codes | Display Only | Yes | Displays the diagnosis code version currently being used. At this time, the only option is ICD-10 and this option will be selected by default. |
| Apply Hawaii General Excise Tax | Checkbox | No | If checked, the Hawaii General Excise Tax is applied to claim totals in charge entry. |