Overview
| Panel | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||
|
(Click an image below to enlarge.)
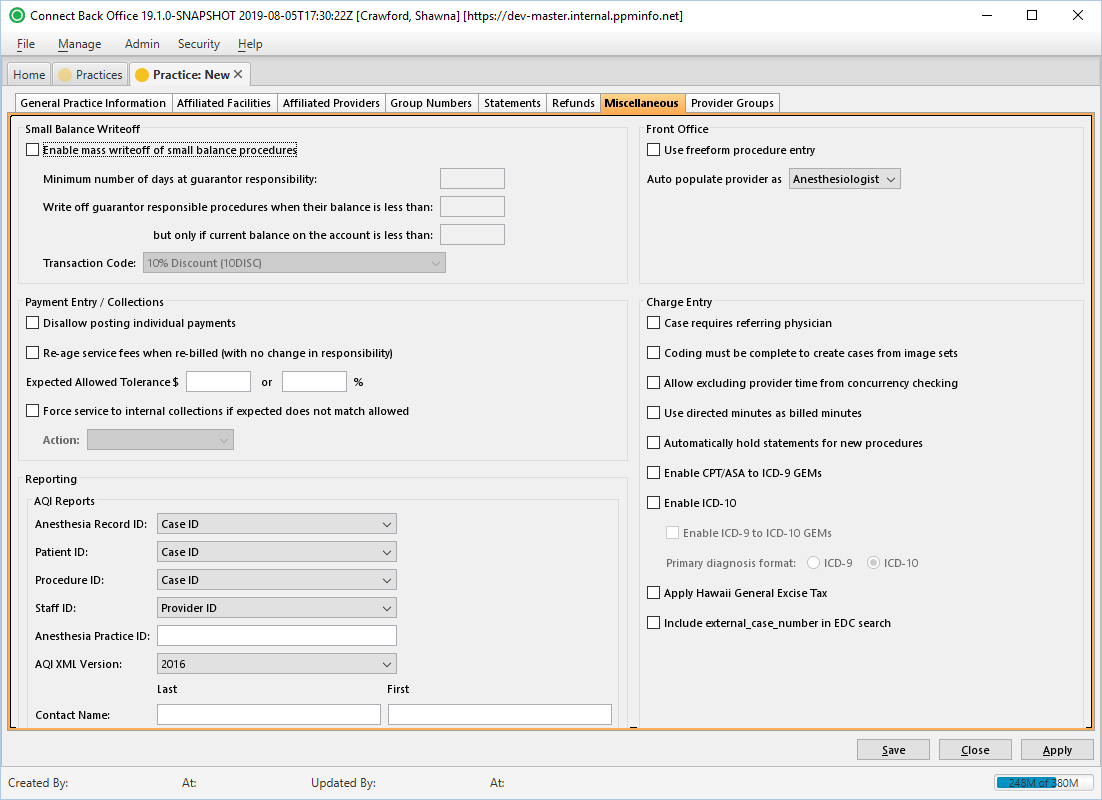
Practice: New Page / Miscellaneous Tab
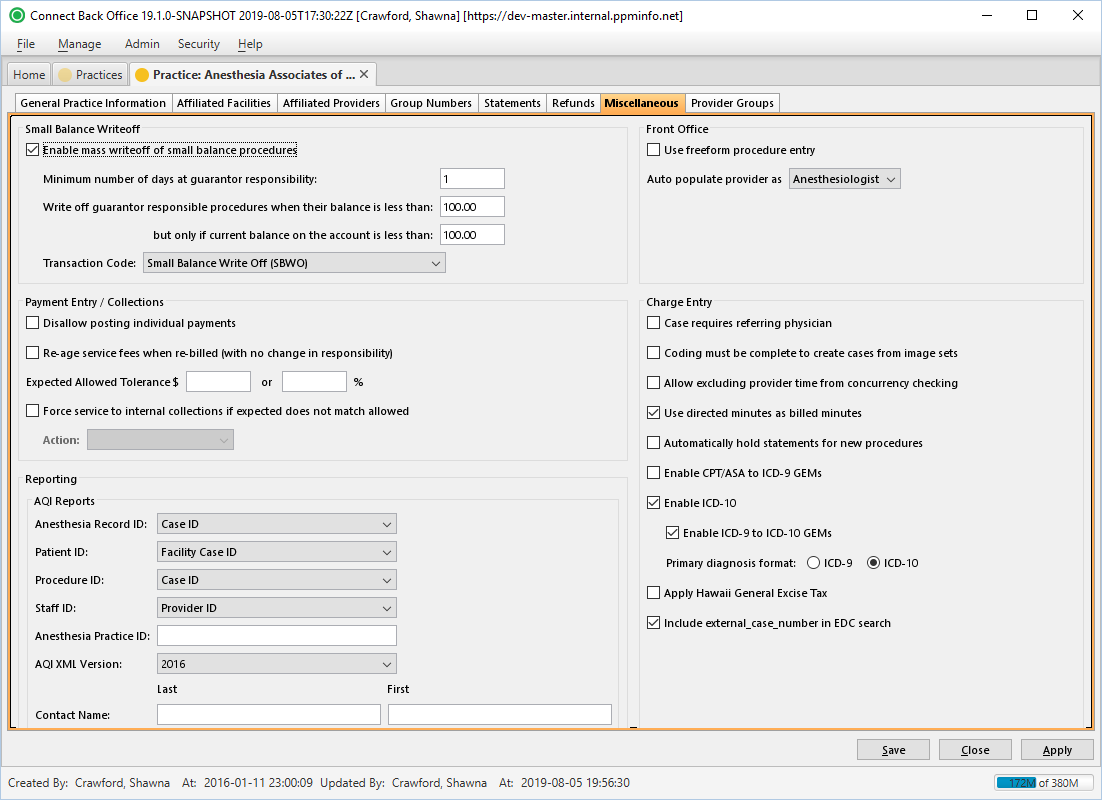
Practice: [name] Page / Miscellaneous Tab
Field Definitions
Field | Type | Required | Description |
| Small Balance Writeoff Section | |||
| Enable mass writeoff of small balance procedures | Specifies criteria for automatically writing off small balances that originated from a procedure. A small balance must meet all of the following criteria to be eligible for writeoff:
The drop down box specifies what Transaction Code the small balance writeoff is posted under. | ||
| Minimum number of days at guarantor responsibility | |||
| Write off guarantor responsible procedures when their balance is less than | |||
| But only if current balance on the account is less than | |||
| Transaction Code | Drop Down | ||
| Payment Entry / Collections Section | |||
| Disallow posting individual payments | Prevents the posting of individual payments within a payment batch. When this option is selected, payments may only be posted from the Payment Batches page. This option is available only when the Payment Batch: [ID] > Expected Count and Expected Total values match what was entered during payment entry. | ||
| Re-age service fees when re-billed (with no change in responsibility) | Resets the responsible balance date to the rebill date, given that responsibility remains the same (guarantor to guarantor, primary to primary, etc.). Unchecking the option will continue to recognize the original bill date as the responsible balance date. Only option checked by default. | ||
| Expected Allowed Tolerance | Specifies the over-under criteria the Actual Allowed amount an EOB must exceed beyond the Expected Allowed meet for inclusion in the Payment Exceptions Report, which is generated from the Payment Batch [ID] page in Back Office. If an Actual Allowed amount from an EOB either exceeds the set thresholds, the amounts entered in these fields will determine if the payment is included in the report. You may enter either a dollar amount or a percentage (of the total expected allowed amount). If both values are entered, the inclusion in the report will be decided based on the lesser amount. Example: Tolerance is set to $5.00 or 1%. Expected allowed for procedure 99213 is $100.00. We would return two values as a tolerance for the above: $5.00 and $1.00 (100 x .01), so we would return this on the report if the actual allowed entered is $98.99 or $101.01, because the percentage is the lesser of the two. | ||
| Force service to internal collections if expected does not match allowed | Forces service fee lines that are outside of the Expected Allowed Tolerance range to internal insurance collections and the action type assigned via the drop-down box is initiated. This functionality is similar to checking the Collections check box in the current payment entry environment. Examples (given that the allowed amount is outside of the Expected Allowed Tolerance limits): 1. The practice expects $1,000 from Primary Payer 1 for Service X. Primary Payer 1 allows $800. Service (fee line) X is automatically moved to internal insurance collections and the default Action Type indicated on the Miscellaneous tab is initiated for Primary Payer 1. 2. The practice expects $1,000 from Primary Payer 1 for service X. The primary payer allows $1,500. Service (fee line) X is automatically moved to internal insurance collections and the default Action Type indicated on the Miscellaneous tab is initiated for Primary Payer 1. Since $1,500 pays the practice more than expected, sending the service fee line to internal insurance collections is a means to notify the practice that the allowance should be investigated.
To enable the Action Type drop down, check the Force service to internal collections if expected does not match allowed box. | ||
| Action Type | |||
| Front Office Section | |||
| Use freeform procedure entry | Allows freeform typing in the Procedure field, which is located on the New Patient/Provider Appointment window in Front Office. Checking this option prevents the Procedure drop-down list from appearing. | ||
| Auto populate provider as | Drop Down | Choosing Anesthesiologist will cause the Anesthesiologist field in the New Provider Appointment window to auto-populate with a list of practice providers and can-schedule providers. The Primary Surgeon field will auto-populate with a list of referring physicians. Choosing Primary Surgeon will cause the Primary Surgeon field in the New Provider Appointment window to auto-populate with the list of practice providers and can-schedule providers. The Anesthesiologist field will auto-populate with the list of referring physicians. This option was previously located in Front Office. | |
| Charge Entry Section | |||
Case requires referring physician | Designates the Referring Physician field as required in Back Office | ||
Coding must be complete to create cases from image sets | Blocks the creation of a case from an image set in Back Office before the Coding form is completed in Image Batches of Back Office. By default, this option is not selected. To restrict cases from being created from image sets before the Coding status is complete, check the box. To allow cases from image sets regardless of the Coding status, leave the check box blank. | ||
Allow excluding provider time from concurrency checking | Allows users of Connect Back Office to check the "Exclude (provider time segment) from concurrency checking when using the Add/Update Provider Time form in charge entry. Excluded minutes will continue to be considered in total case time and start/stop time. When a time segment is excluded, a pop-up alert appears. | ||
Use directed minutes as billed minutes | Uses the directed provider's minutes as the billed minutes for the purpose of calculating directed provider billed minutes and time units. Example Case: | ||
Automatically hold statements for new procedures
| Hold statements for all new cases and procedures at the practice level. Once this box is checked, Connect Back Office will automatically check the Hold Statement box in charge entry on all new procedures. The charge entry Hold Statement option will also automatically become unavailable to the user until the box is unchecked. When held procedures are highlighted in charge entry, an indicator appears in the Procedure Details area (click the link to the left to view an example). | ||
Enable CPT/ASA to ICD-9 GEMs (General Equivalence Mappings) | Populates ICD-9 Code line in Back Office Charge Entry (Add/Update Procedure dialog box) with potential diagnosis code matches based on the CPT code(s) entered. By default, this option is not checked. | ||
Enable ICD-10 | Enables the ICD-10 fields and drop downs in Back Office Charge Entry (Add/Update Procedure dialog box). By default, this option is not checked.
| ||
| Enable ICD-9 to ICD-10 GEMs (General Equivalence Mappings) | Populates mapping options between ICD-9 and ICD-10 diagnosis codes. By default, this option is not checked. This functionality works both ways (ICD-9 to ICD-10 and ICD-10 to ICD-9), depending on the Primary diagnosis format selected (see below). For example, if ICD-9 is selected as the Primary diagnosis format and an ICD-9 Code is selected, the GEM Scenario and Choice Selection dialog box appears and allows the user to choose an ICD-10 code or codes to map to. If the Enable CPT to ICD-9 GEMs is unchecked and the ICD-9 code entered is not associated with the Procedure (CPT) code, an error will advise the user that the ICD-9 code is not associated with the CPT. If ICD-10 is set a the Primary diagnosis format, the Enable CPT to ICD-9 GEMs option does not function, regardless of whether it is checked. The system will instead identify only ICD-9 Code crosswalks for the selected ICD-10 Code. | ||
| Primary diagnosis format | Determines the ICD code set (9 or 10) that displays in the primary position (left side of the ICD code area). It also determines how the Enable ICD-9 to ICD-10 GEMs and Enable CPT to ICD-9 GEMs behave (see above). | ||
| Apply Hawaii General Excise Tax |