Overview
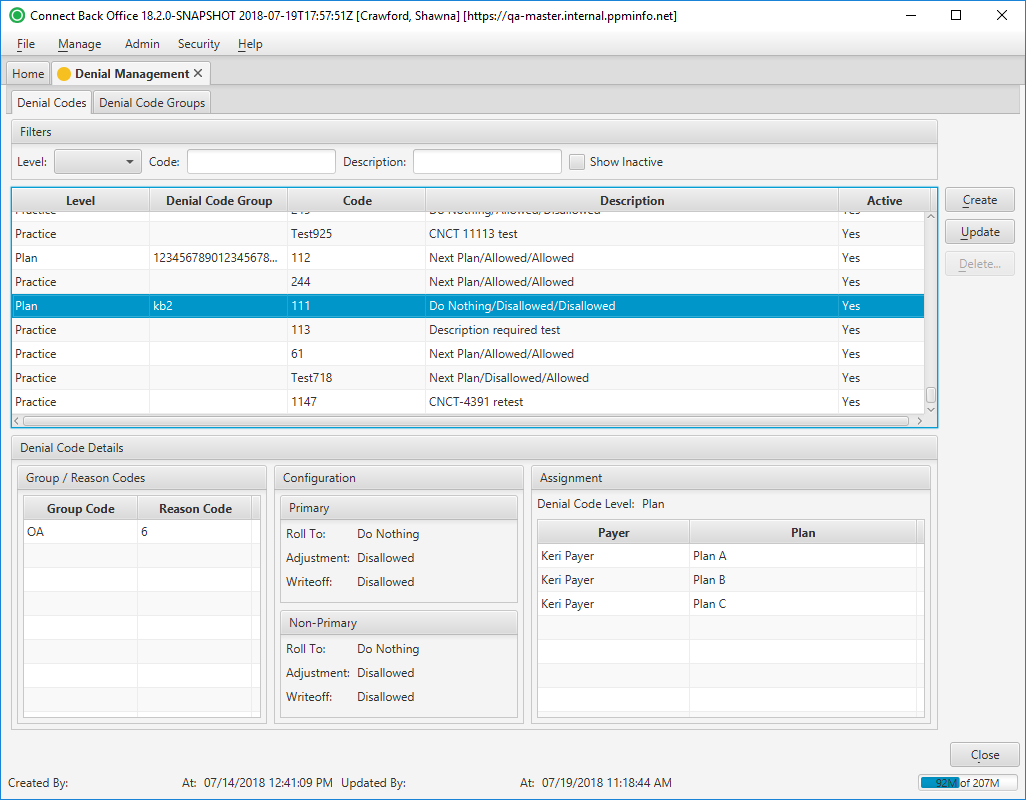
The Denial Management page contains two tabs:
The Denial Codes tab lists the adjustment and denial rules that are applied to group and reason codes used in Connect Back Office. The user rules are added to this page through the Denial Code page.
The Denial Code Groups tab lists the code groupings as set up and defined by the user in tying together two or more denial codes, for ease of selection and application on payments.
Field Definitions
Field | Type | Required | Description |
|---|---|---|---|
| Filters | Filter | No | Allows the list of denial codes to be filtered by Level, Code, and/or Description. Selecting an option from the Level drop down list will limit the denial codes displayed. As you type in the Code and/or Description fields, the payers and plans in the list are filtered to show only those that match what is typed. To restore the list to all payers and plans, clear the contents of the filters. |
| Show Inactive | Checkbox | No | Allows the list of denial codes to be filtered by Active / Inactive. The list defaults to only displaying Active codes, but can be updated to include Inactive codes if the checkbox is selected. |
| Level | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The categorization of the denial code.
|
| Denial Code Group | Display Only (Pulled from created/updated Denial Management rules.) | No | The name of the denial code grouping assigned to the adjustment and denial rule. |
| Code | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The name, or up to 10-character code, of the adjustment and denial rule. System adjustment and denial rules have a prefix of RC. |
| Description | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The description of the adjustment and denial rule. |
| Active | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The current status of the adjustment and denial rule. |
| Denial Code Details Section | |||
| Group / Reason Codes | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The group and reason codes associated to the adjustment and denial rule for communicating from one payer to another why a claim was not paid as billed. For example, PR (Patient Responsibility) is a group code that can have a reason code of 1, indicating that the amount of the adjustment is due to a deductible requirement. |
| Configuration | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The breakdown of the adjustment and denial rule for Primary and Non-Primary payments, including the selections for:
|
| Roll To | Read-only | Yes | The adjustment and denial rule for rolling financial responsibility to the next party when the associated group and reason code is used in Connect Back Office. The Roll To options are defined as follows:
|
| Adjustment | Display Only (Pulled from created/updated Denial Management rules.) | Yes | Indicates whether an adjustment is allowed.
|
| CWOFF | Display Only (Pulled from created/updated Denial Management rules.) | Yes | This option indicates whether a contractual writeoff is allowed for the adjustment and denial rule.
|
| Assignment | Display Only (Pulled from created/updated Denial Management rules.) | Yes | The description of the rule level. If the adjustment and denial rule is at the System level, it will list it as System. If the adjustment and denial rule is at the Practice, Payer, or Plan level, it will list the practice(s), payer(s), or plan(s) to which it applies. |
| Statement Label | Display Only (Pulled from created/updated Denial Management rules.) | No | The text that appears on the statement when the adjustment and denial rule is used in Connect Back Office. If not populated, the contents of the Name field is used. This information is entered in the Statement Label option on the Denial Code window. Populate this field if you do not want the system reason to default to the statements. |
Button Descriptions
Button | Shortcut Keys | Description | Step-By-Step Guides |
|---|---|---|---|
| Create | [Alt] + [C] | Opens the Denial Code window where you can define user adjustment and denial rules for a practice, payer, or plan. | Creating Denial Management Rules |
| Update | [Alt] + [U] | Opens the Denial Code window where you can modify a user adjustment and denial rule, or inactivate / add a statement label to a system adjustment and denial rule. | Updating Denial Management Rules |
| Delete | [Alt] + [D] | Deletes adjustment and denial rules from the master list. System adjustment and denial rules cannot be deleted. |