Overview
The Denial Code page is used to manage the adjustment and denial rules that determine the behavior of group and reason codes used in Connect Back Office. Use the Denial Code page to add or modify user-defined rules that are associated to the HIPAA-compliant reason and group codes, to define a statement label, to assign it to a denial code group, or to inactivate a system adjustment and denial rule.
The adjustment and denial rule determines how financial responsibility roll to, adjustments, and contractual writeoffs are handled for group and reason codes.
The Denial Code page is divided into two tabs:
- Primary
- Non-Primary
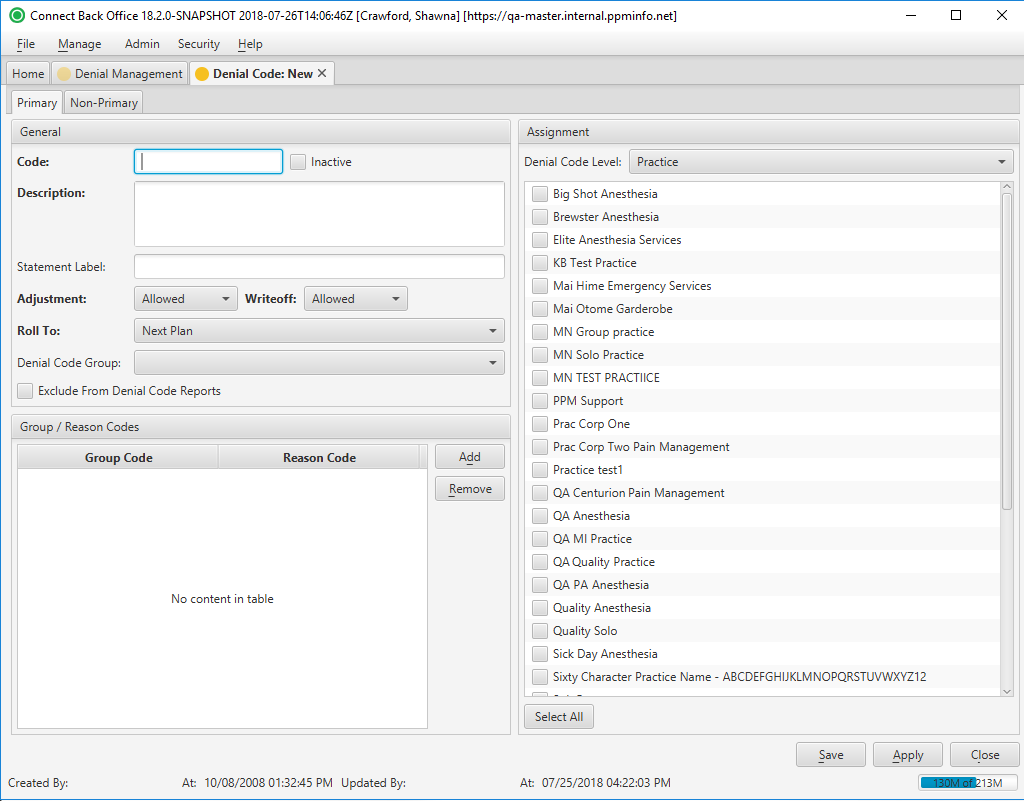
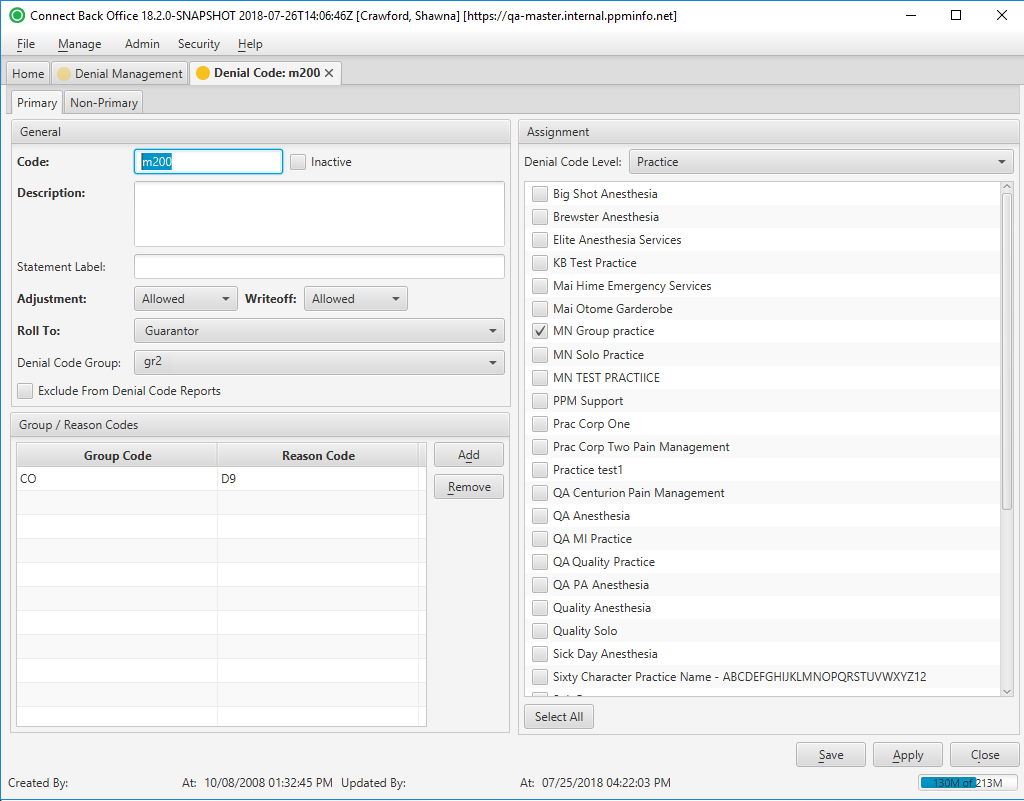
The Primary tab is used to define adjustment and denial rules for primary payments.
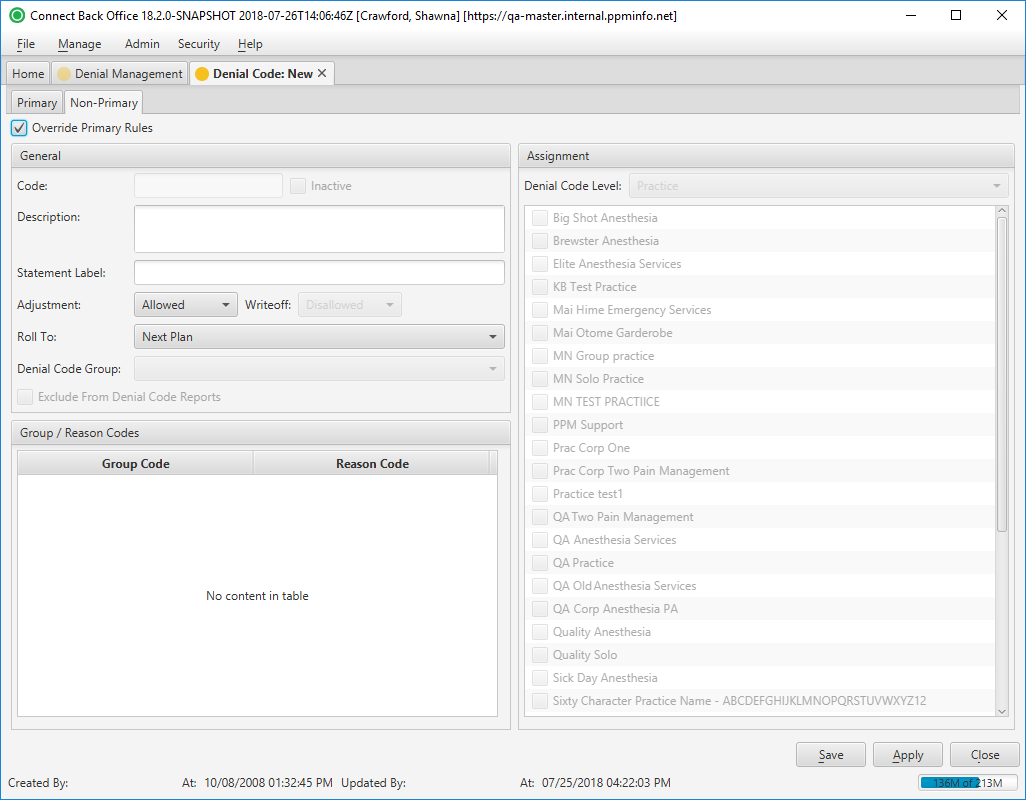
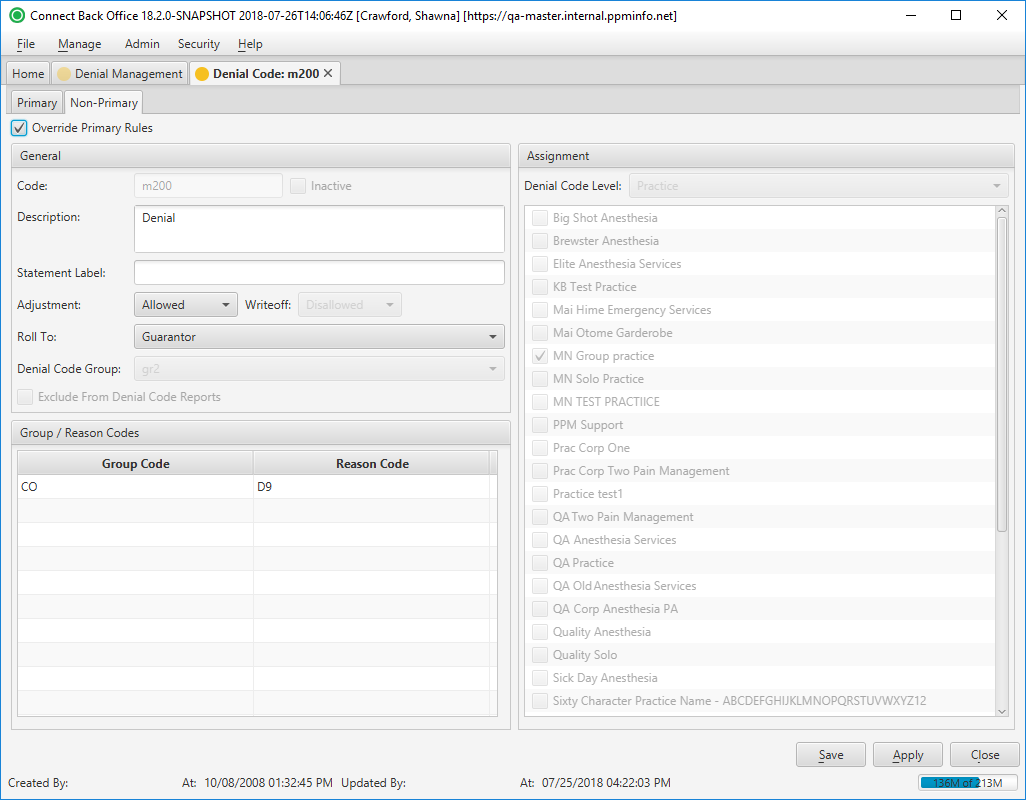
The Non-Primary tab is used to define adjustment and denial rules for non-primary (secondary) payments.
(Click an image below to enlarge.)
Denial Code: New Page / Primary Tab
Denial Code: New Page / Non-Primary Tab
Denial Code: [name] Page / Primary Tab
Denial Code: [name] Page / Non-Primary Tab
Field Definitions
Primary Tab
Field | Type | Required | Description | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General Section | |||||||||||||||
| Code | Free Text | Yes | The 1 to 10-character transaction code that identifies the adjustment and denial rule associated with the adjustment reason and denial codes used by payers to inform members why a claim was adjusted or denied. You cannot change the code on a system adjustment and denial rule. Adjustment and denial rules determine the behavior of the group and reason codes that payers use to explain why a claim was not paid and the action that was taken, adjustment or contractual writeoff. The group and reason codes are HIPPA compliant and are specific to electronic claim filing. These codes are essential to the payment entry function for processing secondary claims correctly. Adjustment and denial rules can be defined for the plan, payer, or practice. The adjustment and denial rule assigned to the practice are used as the default adjustment and denial rules for all payers and plans. The adjustment and denial rule assigned to a plan overrides the payer and the practice. The adjustment and denial rule assigned at the payer overrides those assigned to the practice. | ||||||||||||
| Inactive | Checkbox | Yes | Indicates the status of the adjustment and denial rule. By default, this option is set to No.
| ||||||||||||
| Description | Free Text | Yes | The description of the adjustment and denial rule. You cannot change the description of a system adjustment and denial rule. | ||||||||||||
| Statement Label | Free Text | No | Text that appears on the statement when the adjustment and denial rule is used in Connect Back Office. | ||||||||||||
| Adjustment | Drop Down | Yes | Indicates whether an adjustment is allowed or disallowed when the adjustment and denial rule is applied in Connect Back Office. By default, this option is set to Allowed.
| ||||||||||||
| Writeoff | Drop Down | Yes | Indicates whether a contractual writeoff is allowed or disallowed when the adjustment and denial rule is applied in Connect Back Office. By default, this option is set to Allowed.
| ||||||||||||
| Roll To | Drop Down | Yes | The rule for rolling financial responsibility when this adjustment and denial rule is used in Connect Back Office. Select one of the following options to specify the next party who is responsible for paying the claim:
When multiple group and reason codes have different adjustment and denial rules, the most conservative roll to rule is used. For example, suppose a payer uses two group and reason codes to adjust the payment amount on a claim. One group and reason code has an adjustment and denial rule with the Roll To rule of Next Plan and the other group and reason code has an adjustment and denial rule with a Roll To rule of Do Nothing. The adjustment and denial rule with the Roll To rule of Do Nothing will be applied to the payment because it is the most conservative rule. You can override this rule at the time of payment entry or in the guarantor account, where responsibility can be reassigned via Roll To in Active AR. | ||||||||||||
| Denial Code Group | Drop Down | No | The name of the denial code grouping assigned to the adjustment and denial rule. The list of drop down options is pulled from the Denial Management / Denial Code Groups tab. | ||||||||||||
| Exclude from Denial Code Reports | Checkbox | No | If checked, any denials associated with the denial code will not be included in any denial code reports, e.g., Insurance Payment Denial Detail report. | ||||||||||||
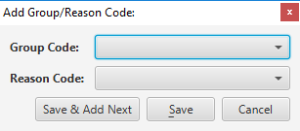
| Group/Reason Codes Section | The group and reason codes associated to the adjustment and denial rule for communicating from one payer to another as to why an adjustment or write-off is being taken. For example, PR (Patient Responsibility) is a group code that can have a reason code of 1, indicating that the amount of the adjustment is due to a deductible requirement. The group and reason codes are used in the Claim Adjustment Reason Codes option in payment entry of Connect Back Office. | ||||||||||||||
| Group Code | Display Only (Pulled from created/updated Group/Reason Code.) | Yes | Associated to the adjustment or writeoff that is being applied to the claim by the payer. The following options are available:
| ||||||||||||
| Reason Code | Display Only (Pulled from created/updated Group/Reason Code.) | Yes | Identifies the claim adjustment. The CSMA code associated with the group code, indicating the reason the claim is being adjusted or denied by the payer. This HIPAA group and reason codes are specific to electronic claims and communicate from one payer to another the reason the claim was not paid as it was billed. If the claim is being adjusted, the reason code is provided on the EOB or remittance advice. | ||||||||||||
| Assignment Section | |||||||||||||||
| Denial Code Level | Drop Down | Yes | These options determine the level to which the adjustment and denial rule is assigned: practice, payer, or plan. This information is required. By default, this option is set to Practice. Adjustment and denial rules are assigned hierarchically by practice, payer, or plan. Payer and plan adjustment and denial rules override adjustment and denial rules at the practice, and the adjustment and denial rules at the plan override the adjustment and denial rules at the payer.
|
Non-Primary Tab
The Non-Primary tab is used to define the adjustment and denial rule for the non-primary payment. It is a copy of Primary tab content, but can be updated as needed for the non-primary payment.
Field | Type | Required | Description | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Override Primary Rules | Checkbox | No | If checked, the Non-Primary tab, and associated rule, is enabled. If enabled, the non-primary rule is applied to non-primary payments. If not checked, the Primary tab rule is applied to all payments, primary and secondary. | ||||||||||||
| General Section | |||||||||||||||
| Code | Free Text | Yes | The 1 to 10-character transaction code that identifies the adjustment and denial rule. The field cannot be edited on the Non-Primary tab. | ||||||||||||
| Inactive | Checkbox | Yes | Indicates the status of the adjustment and denial rule. The field cannot be edited on the Non-Primary tab. | ||||||||||||
| Description | Free Text | Yes | The description of the adjustment and denial rule. You cannot change the description of a system adjustment and denial rule. | ||||||||||||
| Statement Label | Free Text | No | Text that appears on the statement when the adjustment and denial rule is used in Connect Back Office. | ||||||||||||
| Adjustment | Drop Down | Yes | Indicates whether an adjustment is allowed or disallowed when the adjustment and denial rule is applied in Connect Back Office. By default, this option is set to Allowed.
| ||||||||||||
| Writeoff | Drop Down | Yes | Contractual writeoffs are not allowed for non-primary payments. The field is not enabled on the Non-Primary tab. | ||||||||||||
| Roll To | Drop Down | Yes | The rule for rolling financial responsibility when this adjustment and denial rule is used in Connect Back Office. Select one of the following options to specify the next party who is responsible for paying the claim:
When multiple group and reason codes have different adjustment and denial rules, the most conservative roll to rule is used. For example, suppose a payer uses two group and reason codes to adjust the payment amount on a claim. One group and reason code has an adjustment and denial rule with the Roll To rule of Next Plan and the other group and reason code has an adjustment and denial rule with a Roll To rule of Do Nothing. The adjustment and denial rule with the Roll To rule of Do Nothing will be applied to the payment because it is the most conservative rule. You can override this rule at the time of payment entry or in the guarantor account, where responsibility can be reassigned via Roll To in Active AR. | ||||||||||||
| Denial Code Group | Drop Down | No | The name of the denial code grouping assigned to the adjustment and denial rule. The field cannot be edited on the Non-Primary tab. | ||||||||||||
| Exclude from Denial Code Reports | Checkbox | No | If checked, any denials associated with the denial code will not be included in any denial code reports. The field cannot be edited on the Non-Primary tab. | ||||||||||||
| Group/Reason Codes Section | The group and reason codes associated to the adjustment and denial rule for communicating from one payer to another as to why an adjustment or write-off is being taken. For example, PR (Patient Responsibility) is a group code that can have a reason code of 1, indicating that the amount of the adjustment is due to a deductible requirement. The group and reason codes are used in the Claim Adjustment Reason Codes option in payment entry of Connect Back Office. | ||||||||||||||
| Group Code | Display Only (Pulled from created/updated Group/Reason Code.) | Yes | Associated to the adjustment or writeoff that is being applied to the claim by the payer. The following options are available:
The table cannot be edited on the Non-Primary tab. | ||||||||||||
| Reason Code | Display Only (Pulled from created/updated Group/Reason Code.) | Yes | Identifies the claim adjustment. The CSMA code associated with the group code, indicating the reason the claim is being adjusted or denied by the payer. This HIPAA group and reason codes are specific to electronic claims and communicate from one payer to another the reason the claim was not paid as it was billed. If the claim is being adjusted, the reason code is provided on the EOB or remittance advice. The table cannot be edited on the Non-Primary tab. | ||||||||||||
| Assignment Section | |||||||||||||||
| Denial Code Level | Drop Down | Yes | These options determine the level to which the adjustment and denial rule is assigned: practice, payer, or plan. The selection cannot be edited on the Non-Primary tab. Adjustment and denial rules are assigned hierarchically by practice, payer, or plan. Payer and plan adjustment and denial rules override adjustment and denial rules at the practice, and the adjustment and denial rules at the plan override the adjustment and denial rules at the payer.
|
Button Descriptions
Button | Shortcut Keys | Description | Step-By-Step Guides |
|---|---|---|---|
| Add | [Alt] + [D] | To add a group and reason code. |
|
| Remove | [Alt] + [R] | To delete a group and reason code. |
|
| Select All/None | Provides a convenient way to associate/disassociate all records for the selected Denial Code Level. The button toggles between values upon selection. |