Overview
The Eligibility page is comprised of three tabs:
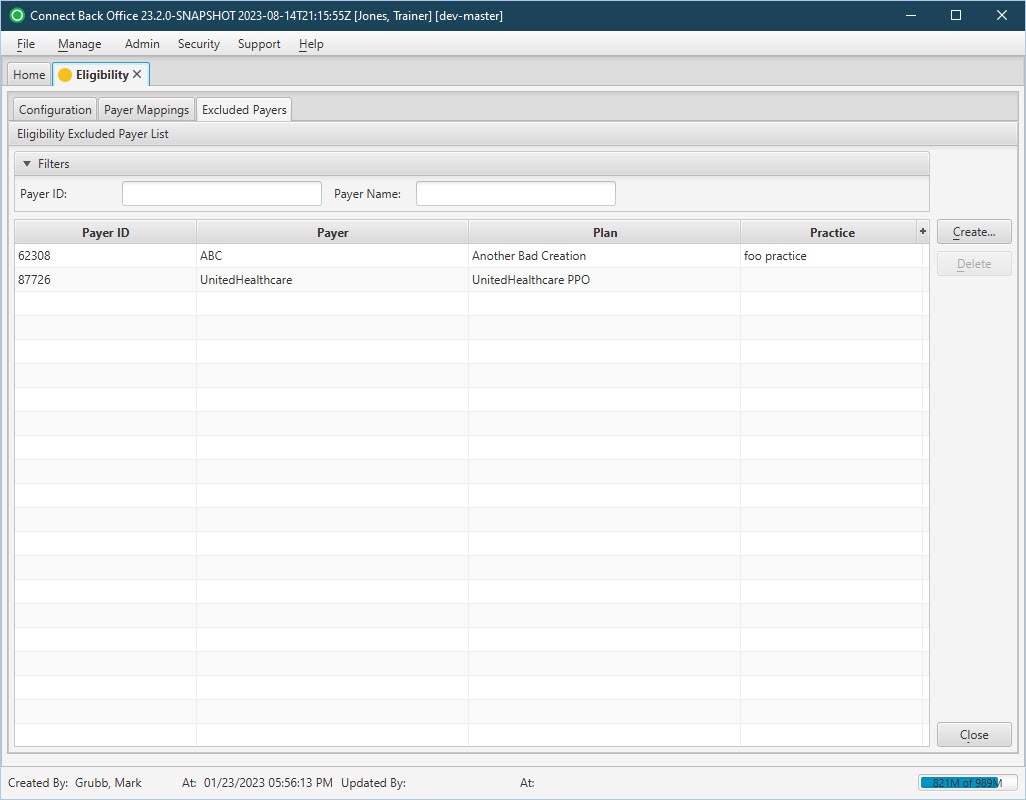
The Eligibility / Excluded Payers tab is used to disable Eligibility checks for certain plans. When Eligibility is disabled, the plan will not display in the mapping tool and will not be included in error reports when Eligibility is run.
Field Definitions
Field | Type | Required | Description |
|---|---|---|---|
| Eligibility Excluded Payer List Section | |||
| Filters | Filter | No | Filtering options used to specify which payers are displayed in the Excluded Payers table. Allows the list of collection information to be filtered by Payer ID and Payer Name. As you type, the list is filtered to show only the data that matches what was typed. To restore the list to all excluded payer information, clear the contents of the filters. |
| Payer ID | Display Only (pulled from created Eligibility Payer Exclusion record) | Yes | The unique payer identification number associated with the selected payer. |
| Payer | Display Only (pulled from created Eligibility Payer Exclusion record) | Yes | The name of the company that owns the plan to which claims are submitted and being excluded from Eligibility checks. |
| Plan | Display Only (pulled from created Eligibility Payer Exclusion record) | No | The name of the plan to which claims are submitted and being excluded from Eligibility checks. |
| Practice | Display Only (pulled from created Eligibility Payer Exclusion record) | No | The name of practice where the payer is being excluded from Eligibility checks. |
Button Descriptions
Button | Shortcut Keys | Description | Step-By-Step Guides |
|---|---|---|---|
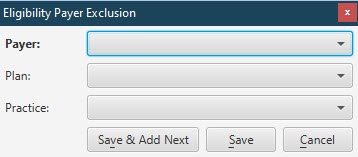
| Create | [Alt] + [C] | To add a new payer to the Excluded Payers (Eligibility check) list. |
The selected Payer/Plan/Practice will be excluded from Eligibility checks. A Payer must be selected for the exclusion. If no Plan and/or Practice is selected, all Plans and/or Practices associated with the Payer will be included in the exclusion. |
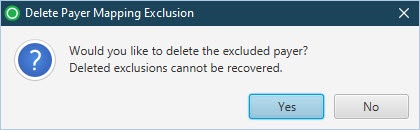
| Delete | [Alt] + [D] | To remove a payer from the Excluded Payers (Eligibility check) list. |
|