Overview
Purpose
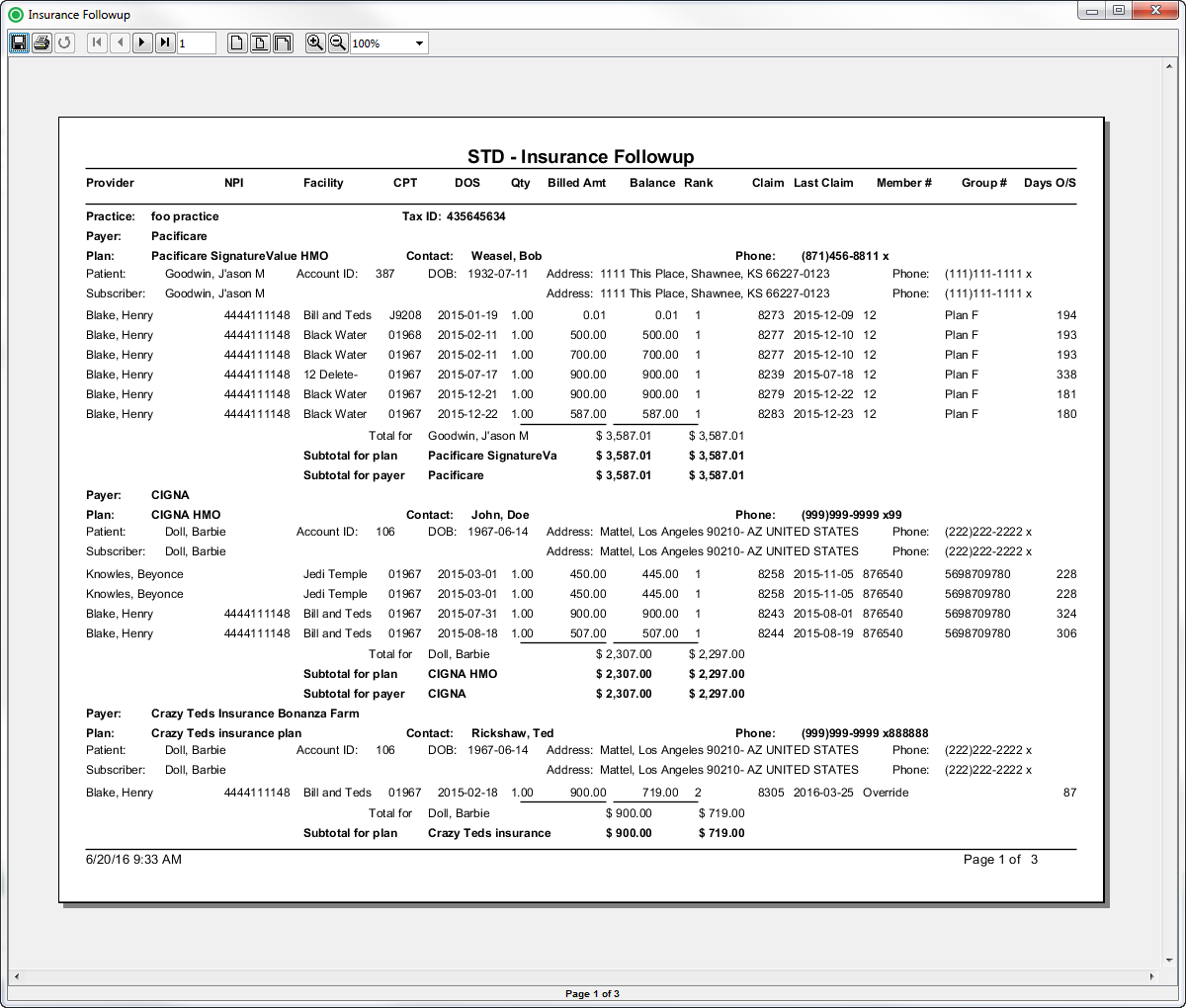
This report is used as a tool to review or work outstanding balances, based on date of service criteria. It identifies unpaid claims by payers so collectors can follow up with payers. The report shows the details of the claims submitted to a specific payer for a particular plan by patient and subscriber. This report includes provider, NPI, facility, procedure code, date of service, quantity, billed amount, current balance, payer rank, claim ID, claim date; member number, group number, and days outstanding.
Category
Management
Type
Detail
Mode
Date of Service
Output Options
View/Print, CSV, Excel, or PDF
Sample Reports
(Click an image to enlarge)
Portal
Back Office
Field Definitions
Field | Calculation Formula | Description |
|---|---|---|
| Account ID | The account number of the guarantor account. | |
Balance | The current balance of the claim. | |
Billed Amount | The amount billed to the payer. | |
| Claim Date | The date that the claim was generated. | |
Claim | The identification number issued to the claim when it was generated. | |
Date of Service | The date the procedure was performed. | |
Days Outstanding | The number of days outstanding since the claim was generated. | |
Facility | The name of the facility where the patient was treated. | |
| Patient ID | The identification number of the patient. | |
| Patient DOB | The date of birth of the patient. | |
| Patient Name | The name of the patient. | |
| Patient Address | The address of the patient. | |
| Payer Rank | The insurance ranking of the payer (1=primary, 2=secondary and 3=tertiary). | |
| Practice | The practice for which the charge is being billed. | |
| Tax ID | UPDATE | |
| Payer | The payer in the practice who has financial responsibility of the outstanding debt. | |
| Plan | The name of the plan to which charges were billed on the case. | |
| Plan Contact | UPDATE | |
| Procedure Code | The (ASA and CPT) procedure codes entered on the case. | |
Quantity | The quantity of the procedure. | |
Rendering Provider | The name of the provider (last name, first name) who performed the procedure on the case. | |
Rendering Provider NPI | The national provider identification number issued to the provider. | |
Subscriber Group Number | The identification number of the group. | |
| Subscriber Member Number | The identification number of the member. | |
| Subscriber Name | The name of the person who is insured. | |
| Subscriber Address | The address of the person who is insured. | |
| Subscriber Phone | The telephone number of the person who is insured. |
Available Report Filters
Option | Type | Required | Description |
|---|---|---|---|
| FIX DATE | UPDATE | ||
Date of Service Begin | Drop Down | Yes | Filters by the beginning date of the date of service for the claims that you want to include in the report. By default, this filter is set to January 01 of the current year, for example,12 -01-01. |
Date of Service End | Drop Down | Yes | Filters by the ending date of the date of service for the claims that you want to include in the report. By default, this filter is set to the current date. |
Practices | List Selection | Yes | Filters by all practices or by one or more practices. By default, this filter is set to All Practices. |
Providers | List Selection | Yes | Filters by all providers or by one or more providers. By default, this filter is set to All Providers. |
Facilities | List Selection | Yes | Filters by all facilities or by one or more facilities. By default, this filter is set to All Facilities. |
Payers | List Selection | Yes | Filters by all payers or by one or more payers. By default, this filter is set to All Payers. |
Financial Class | List Selection | Yes | Filters by one or more of the following options: Commercial, Medicare, Medicaid, Workers Comp, or Self-Pay. |
Plans | List Selection | Yes | Filters by all plans or by one or more plans. By default, this filter is set to All Plans. |
Procedure Categories | List Selection | Yes | Filters by all procedure categories or by one or more procedure categories. By default, this filter is set to All Categories. |