Overview
Purpose
This report analyzes procedure level information for outstanding balances.
Category
Aging
Type
Detail
Mode
Not applicable
Output Options
CSV or Excel
Sample Reports
(Click an image to enlarge)
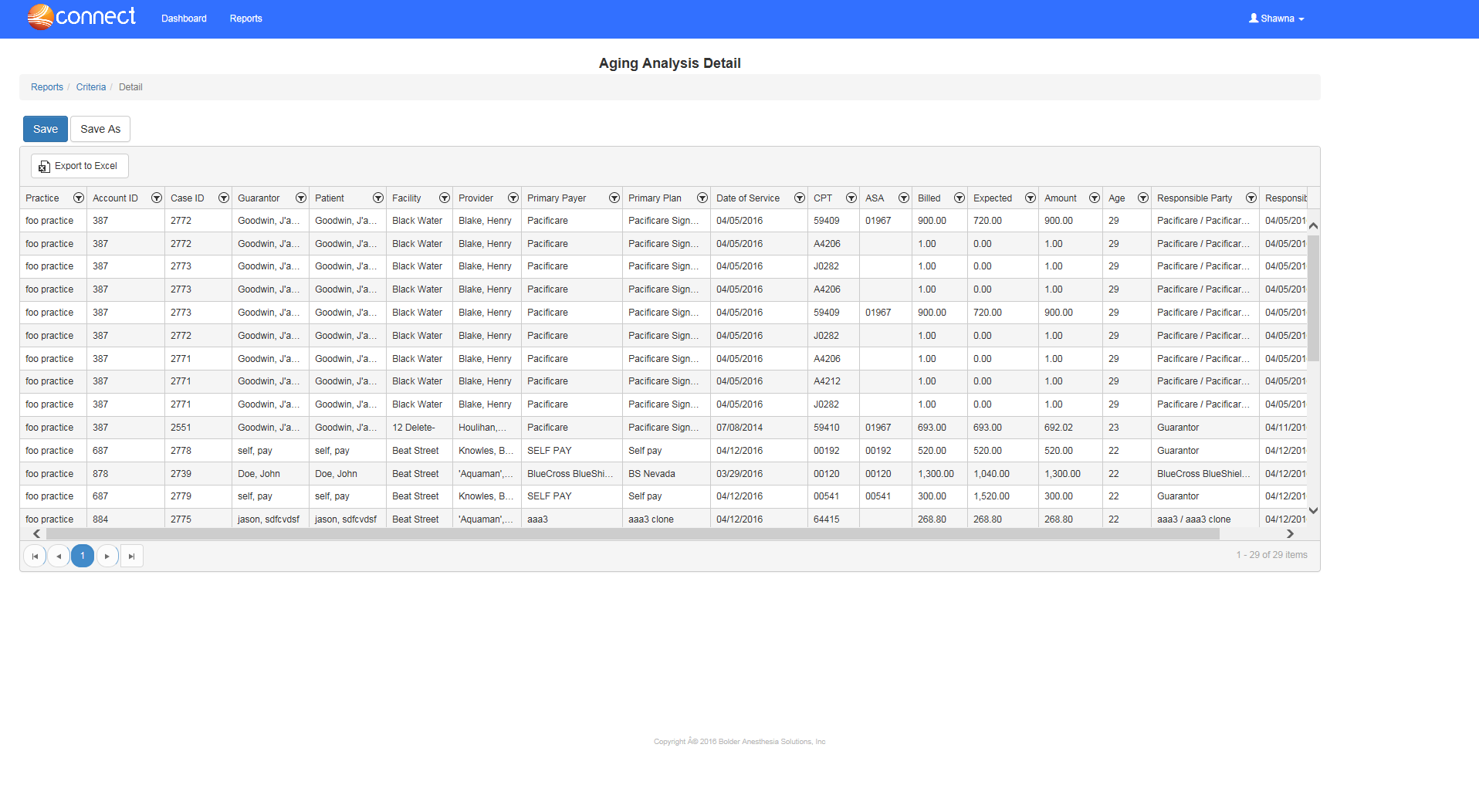
Portal
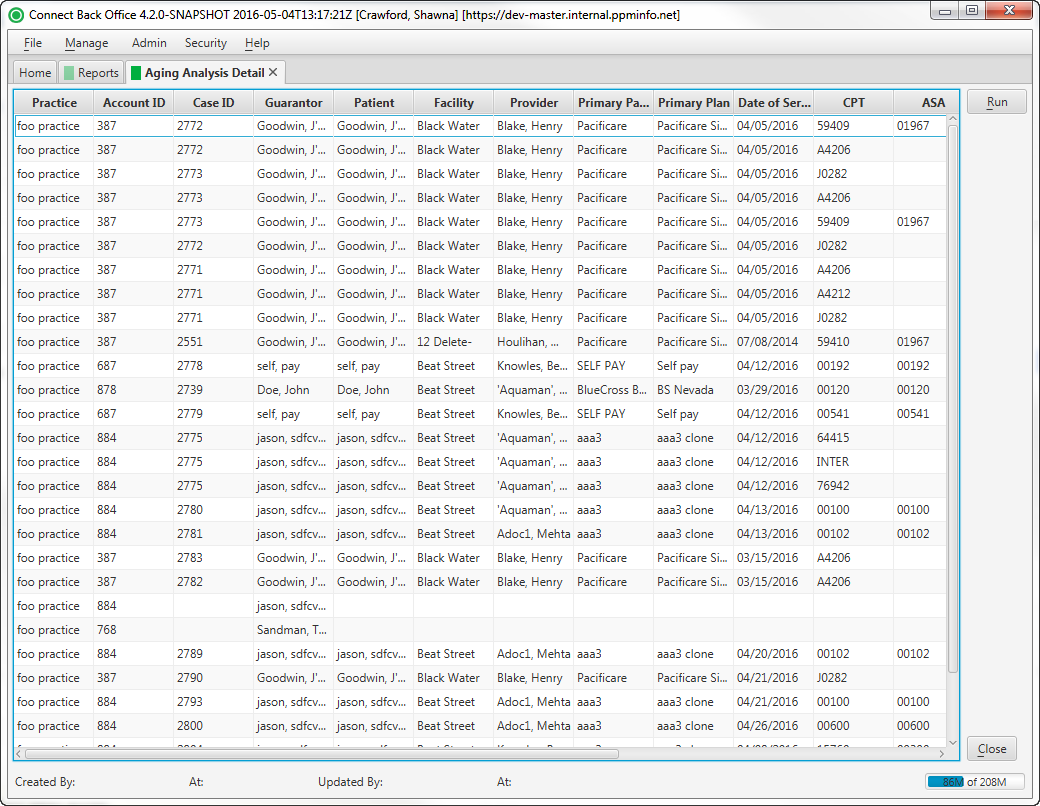
Back Office
Field Definitions
Field | Calculation Formula | Description |
|---|---|---|
| Practice | The practice for which the charge is being billed. | |
| Account ID | The account number of the guarantor account. | |
Case ID | UPDATE | |
| Guarantor | The financially-responsible person or organization on the account. | |
| Patient | The name of the patient on the case. | |
| Facility | The facility where the service was rendered, which is specified on the case in charge entry. | |
| Provider | UPDATE | |
| Primary Payer | UPDATE | |
| Primary Plan | UPDATE | |
| Date of Service | The date that the service was rendered. | |
| CPT | The general procedure code that was entered as the procedure billed on the case in charge entry. | |
| ASA | The anesthesia procedure code that was entered as the procedure billed on the case in charge entry. | |
| Billed | The amount that was billed for total charges for each procedure. | |
| Expected | The expected amount of payment from the responsible party for the amount billed, which is determined by the expected fee schedule configured at the practice configuration. | |
| Amount | The outstanding balance on the account. | |
| Age | The number of days that the account has aged from claim generation to current date. Aging is based on the aging buckets defined in the practice configuration (0 to 30, 31 to 60, 61 to 90, 91 to 120, 121 to 180, over 180). | |
| Responsible Party | The person or payer/plan who is responsible for reimbursement of the charges. | |
| Responsibility Date | The date that the person or payer/plan became financially responsible for the amount billed, for example, guarantor or payer or plan. If a case is re-billed as option 1, this date is the responsibility date of the original case. |
Available Report Filters
Option | Type | Required | Description |
|---|---|---|---|
| Age From | Free Text (Numeric) | Yes | Filters by the number of days specified as the beginning interval. By default, this filter is set to 0 (zero). (0 to 30, 31 to 60, 61 to 90, 91 to 120, 121 to 180, over 180). |
| Age To | Free Text (Numeric) | Yes | Filters by the number of days specified as the ending interval. By default, this filter is set to 30. (0 to 30, 31 to 60, 61 to 90, 91 to 120, 121 to 180, over 180). |
| Practices | List Selection | Yes | Filters by all practices or one or more practices for which there are outstanding balances for procedures performed. By default, this filter is set to All Practices. |
| Providers | List Selection | Yes | Filters by all providers or by one or more providers. By default, this filter is set to All Providers. |
| Facilities | List Selection | Yes | Filters by all facilities or by one or more facilities where services were rendered. By default, this filter is set to All Facilities. |