Overview
| Panel | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
|
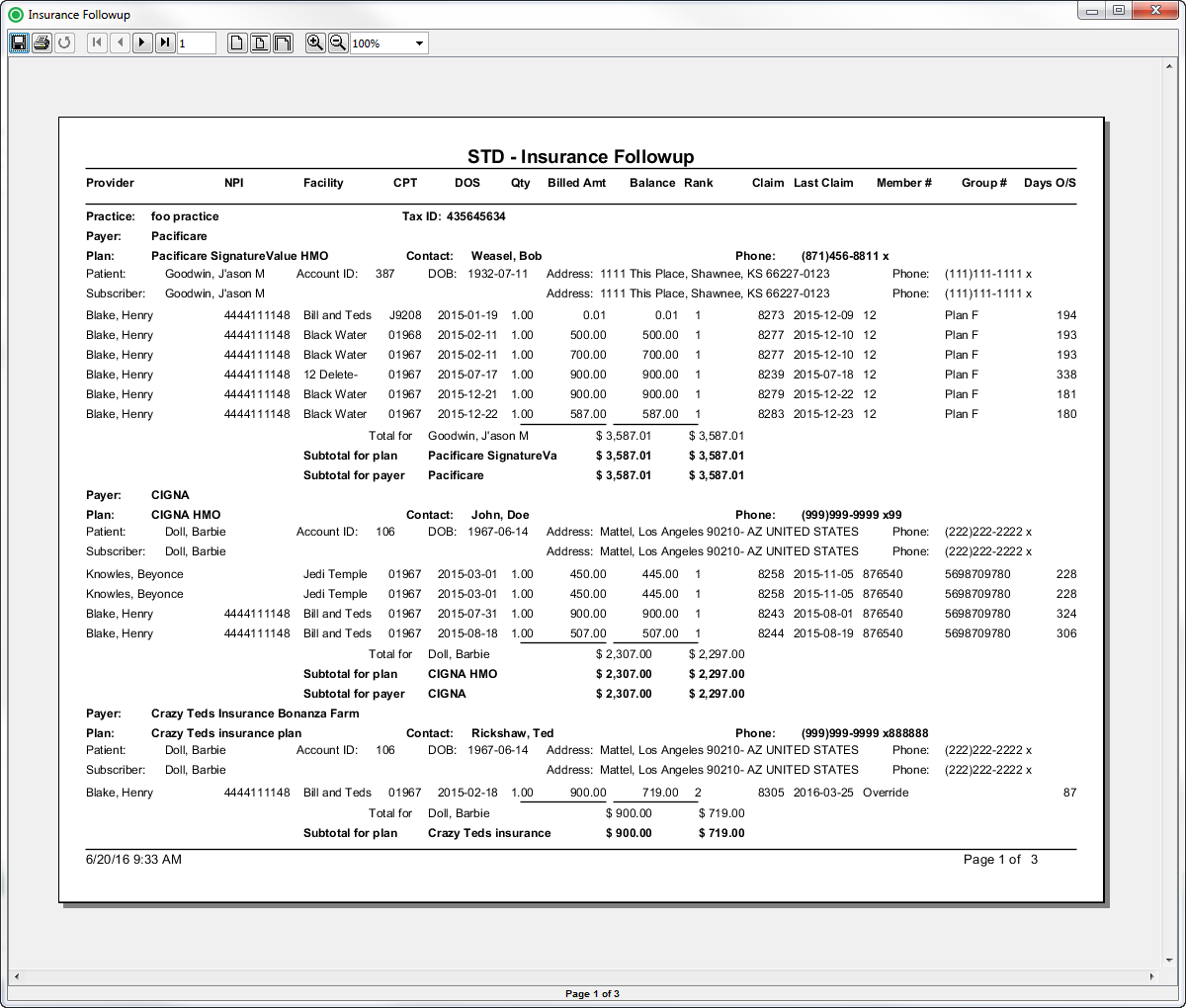
Sample
ReportReports
(Click the Click an image to enlarge)
Back Office
Field Definitions
Field |
|---|
Description |
|---|
Description
Provider
The name of the provider (last name, first name) who performed the procedure on the case.
NPI
The national provider identification number issued to the provider.
| Account ID | The account number of the guarantor account. |
Balance | The current balance of the claim. |
Billed Amount | The amount billed to the payer. |
| Claim Date | The date that the claim was generated. |
Claim | The identification number issued to the claim when it was generated. |
Date of Service | The date the procedure was performed. |
Days Outstanding | The number of days outstanding since the claim was generated. |
Facility |
Facility
The name of the facility where the patient was treated. |
CPT
| Patient ID | The |
| identification number of the |
| patient. |
DOS
| Patient DOB | The date |
Qty
The quantity of the procedure.
Billed Amt
The amount billed to the payer.
Balance
The current balance of the claim.
| of birth of the patient. | |
| Patient Name | The name of the patient. |
| Patient Address | The address of the patient. |
| Payer Rank |
Rank
The insurance ranking of the payer (1=primary, 2=secondary and 3=tertiary). | |
| Practice | The practice for which the charge is being billed. |
| Tax ID | The Tax Identification Number of the associated practice. |
| Payer | The primary insurance payer on the case with financial responsibility for the outstanding debt. |
Claim
The identification number issued to the claim when it was generated.
Last Claim
The date that the claim was generated.
Member #
The identification number of the member.
| Plan | The primary insurance plan on the case to which charges were billed. |
| Plan Contact | The primary contact for the insurance plan. |
| Procedure Code | The (ASA and CPT) procedure codes entered on the case. |
Quantity | The quantity of the procedure. |
Rendering Provider | The name of the provider (last name, first name) who performed the procedure on the case. |
Rendering Provider NPI | The national provider identification number issued to the provider. |
Subscriber Group Number |
Group #
The identification number of the group. |
Days O/S
| Subscriber Member Number |
The |
identification number of the member. | |
| Subscriber Name | The name of the person who is insured. |
| Subscriber Address | The address of the person who is insured. |
| Subscriber Phone | The telephone number of the person who is insured. |
Available Report Filters
Option | Type | Required | Description |
|---|---|---|---|
Date |
| Drop Down | Yes | Filters |
transactions displayed by the selected time period. Options include: Custom Date Range, Last # of Days, Today, Previous Day, Current Month, Previous Month, Current Year, and Previous Year.
| ||
Practices | List Selection |
Date of Service End
Filters by the ending date of the date of service for the claims that you want to include in the report. By default, this filter is set to the current date.
Facilities
| Yes | Filters by all |
practices or by one or more |
practices. By default, this filter is set to All |
Practices. |
Financial Classes
Filters by one or more of the following options: Commercial, Medicare, Medicaid, Workers Comp, or Self-Pay.
| |||
Providers | List Selection | Yes | Filters by all |
providers or by one or more |
providers. By default, this filter is set to All |
Providers. |
Facilities | List |
| Selection | Yes | Filters by all |
facilities or by one or more |
facilities. By default, this filter is set to All |
Facilities. |
Payers | List Selection | Yes | Filters by all |
payers or by one or more |
payers. By default, this filter is set to All |
Payers. | |||
Financial Class | List Selection | Yes | Filters by one or more of the following options: Commercial, Medicare, Medicaid, Workers Comp, or Self-Pay. |
Plans |
| List Selection | Yes | Filters by all |
plans or by one or more |
plans. By default, this filter is set to All |
Plans. |
Procedure Categories | List Selection | Yes | Filters by all |
procedure categories or by one or more |
procedure categories. By default, this filter is set to All |
Categories. |