Overview
|
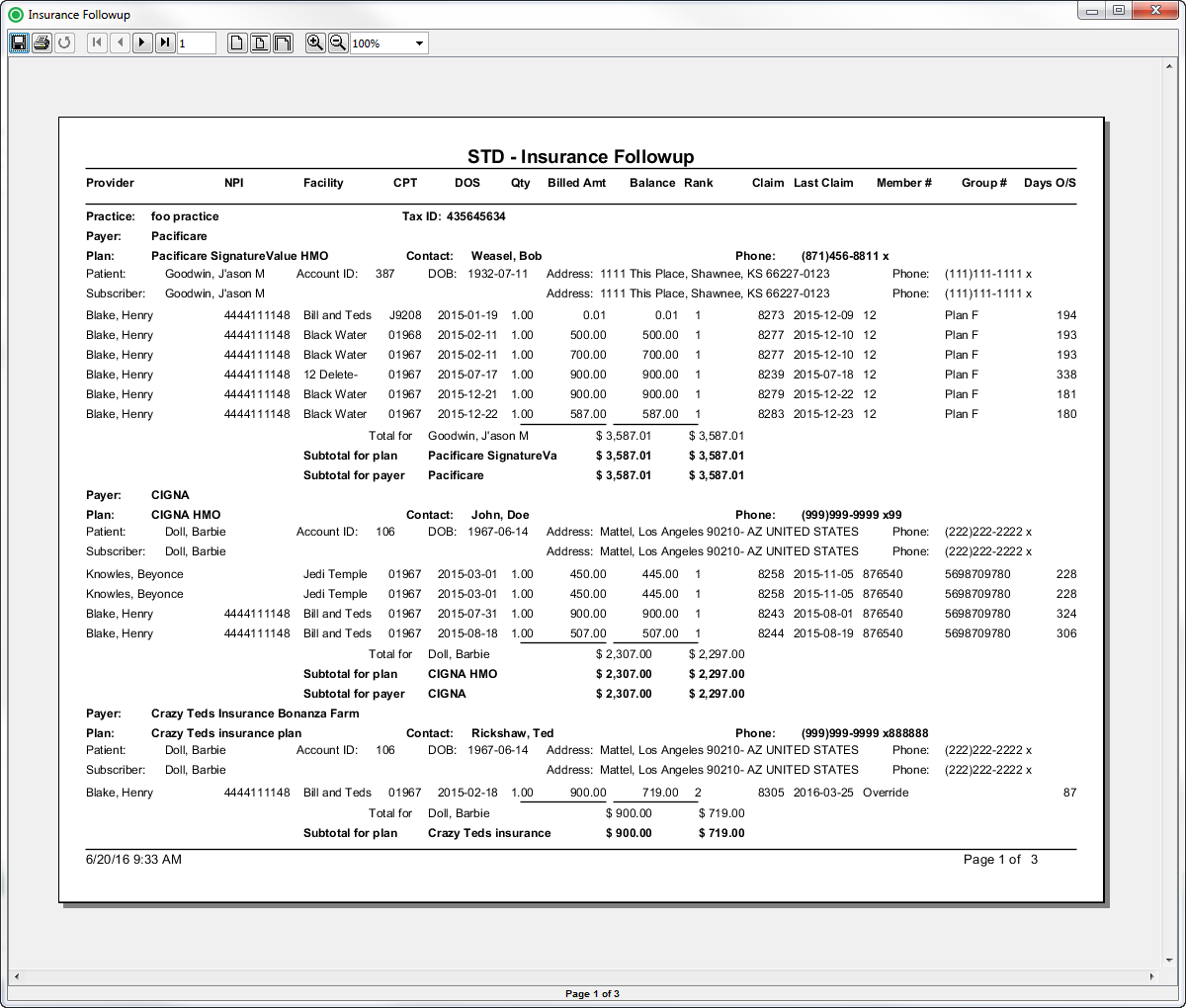
Sample Reports
(Click an image to enlarge)
Back Office
Field Definitions
Field | Description |
|---|---|
| Account ID | The account number of the guarantor account. |
Balance | The current balance of the claim. |
Billed Amount | The amount billed to the payer. |
| Claim Date | The date that the claim was generated. |
Claim | The identification number issued to the claim when it was generated. |
Date of Service | The date the procedure was performed. |
Days Outstanding | The number of days outstanding since the claim was generated. |
Facility | The name of the facility where the patient was treated. |
| Patient ID | The identification number of the patient. |
| Patient DOB | The date of birth of the patient. |
| Patient Name | The name of the patient. |
| Patient Address | The address of the patient. |
| Payer Rank | The insurance ranking of the payer (1=primary, 2=secondary and 3=tertiary). |
| Practice | The practice for which the charge is being billed. |
| Tax ID | The Tax Identification Number of the associated practice. |
| Payer | The primary insurance payer on the case with financial responsibility for the outstanding debt. |
| Plan | The primary insurance plan on the case to which charges were billed. |
| Plan Contact | The primary contact for the insurance plan. |
| Procedure Code | The (ASA and CPT) procedure codes entered on the case. |
Quantity | The quantity of the procedure. |
Rendering Provider | The name of the provider (last name, first name) who performed the procedure on the case. |
Rendering Provider NPI | The national provider identification number issued to the provider. |
Subscriber Group Number | The identification number of the group. |
| Subscriber Member Number | The identification number of the member. |
| Subscriber Name | The name of the person who is insured. |
| Subscriber Address | The address of the person who is insured. |
| Subscriber Phone | The telephone number of the person who is insured. |
Available Report Filters
Option | Type | Required | Description | |
|---|---|---|---|---|
Date | Drop Down | Yes | Filters transactions displayed by the selected time period. Options include: Custom Date Range, Last # of Days, Today, Previous Day, Current Month, Previous Month, Current Year, and Previous Year.
| |
Practices | List Selection | Yes | Filters by all practices or by one or more practices. By default, this filter is set to All Practices.
| |
Providers | List Selection | Yes | Filters by all providers or by one or more providers. By default, this filter is set to All Providers. | |
Facilities | List Selection | Yes | Filters by all facilities or by one or more facilities. By default, this filter is set to All Facilities. | |
Payers | List Selection | Yes | Filters by all payers or by one or more payers. By default, this filter is set to All Payers. | |
Financial Class | List Selection | Yes | Filters by one or more of the following options: Commercial, Medicare, Medicaid, Workers Comp, or Self-Pay. | |
Plans | List Selection | Yes | Filters by all plans or by one or more plans. By default, this filter is set to All Plans. | |
Procedure Categories | List Selection | Yes | Filters by all procedure categories or by one or more procedure categories. By default, this filter is set to All Categories. |