Overview
Purpose
This report analyzes details of payment batch at time of posting.
Category
Management
Type
Detail
Mode
Accounting / Posted
Output Options
CSV or Excel
Sample Reports
(Click an image to enlarge)
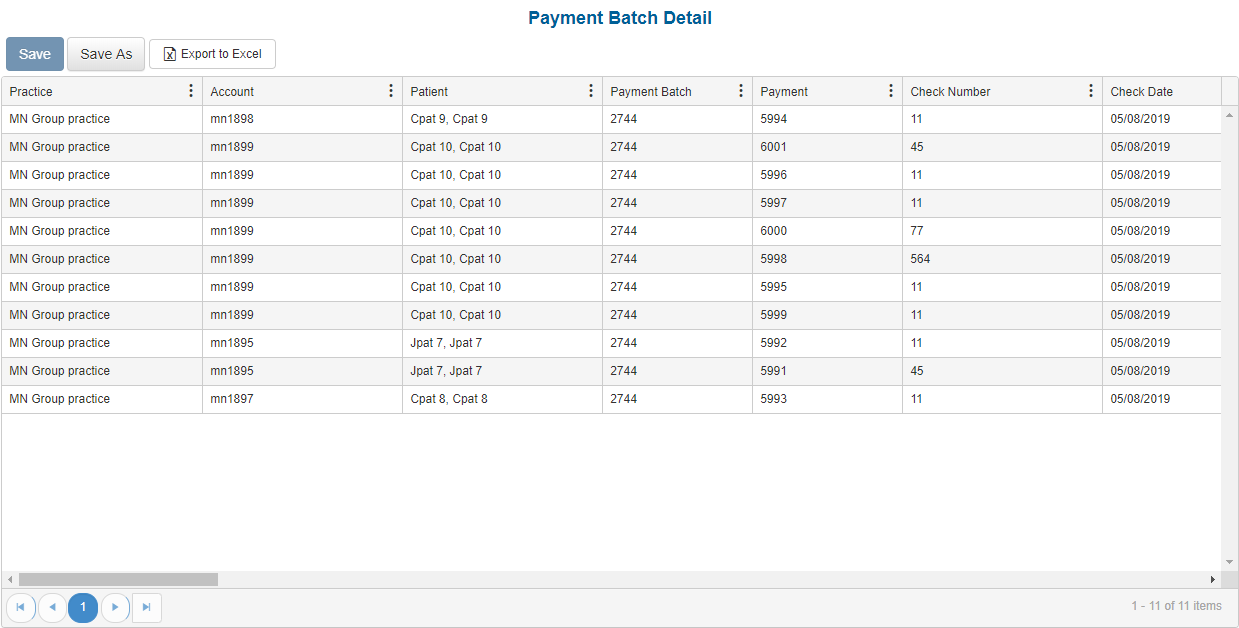
Portal
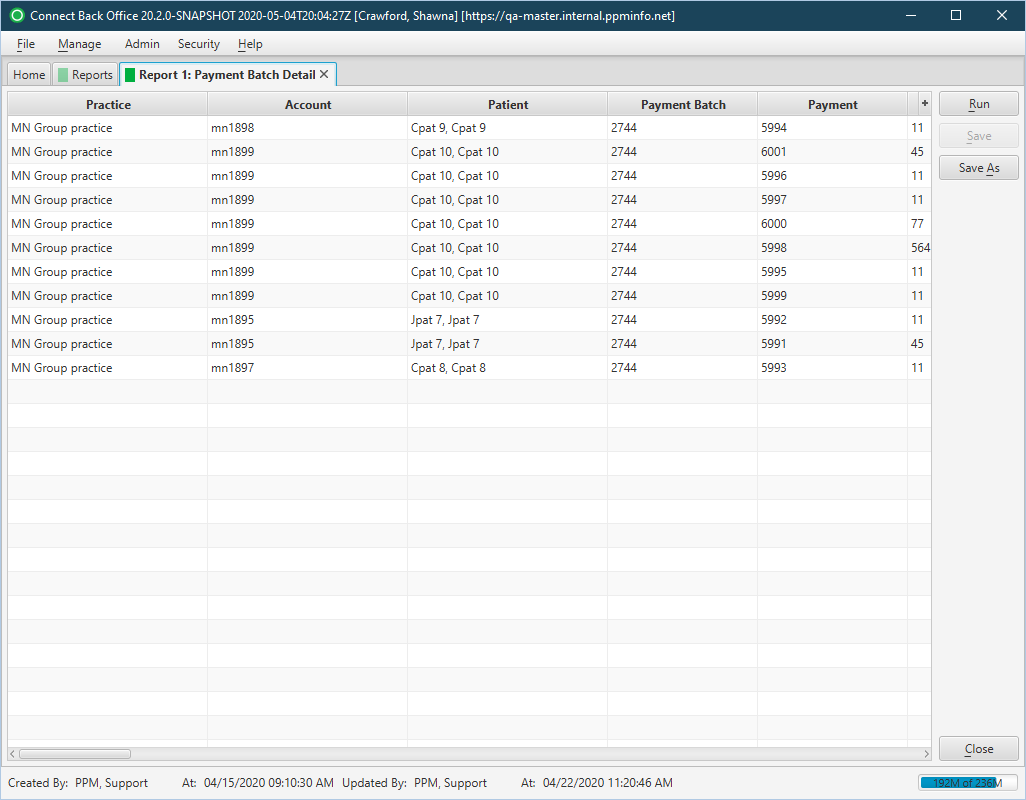
Back Office
Field Definitions
Field | Description |
|---|---|
| Practice | The practice for which the charge is being billed. |
| Account | The account number of the guarantor account. Displays as Account Prefix + Account ID. |
| Patient | The name of the patient on the case. The person treated on the case. |
| Payment Batch | The unique identification number of the payment batch including the payment. |
| Payment | The unique identification number assigned to the payment when it was created. |
| Check Number | The check number of a remitted check. |
| Check Date | The date on the remitted check. |
| Check Amount | The amount of the remitted check. |
| Remitter | The name of the payer, person, or organization that issued the payment. |
| Accounting Date | The accounting date for this payment. |
| Posted Date | The date the transaction was posted to the guarantor account. |
| Claim | The Claim ID to which the insurance payment has been applied. |
| Rendering Provider | The name of the provider (last name, first name middle) who performed the procedure on the case. |
| Referring Provider | The name of the physician(last name, first name middle) who referred the patient. |
| Payer | The primary insurance payer on the case with financial responsibility for the outstanding debt. |
| Plan | The primary insurance plan on the case to which charges were billed. |
| Payment Rank | The rank of the payer when there is one or more payers on the case. By default, this option is set to the primary payer. If the case has multiple payers, you can specify the rank of the payer to which a payment is being applied. |
| Payment Type | The type of payment, as entered during creation of the payment. Values include:
|
| Transaction Type | The type of transaction used for the payment, e.g, credit card, check. |
| Date of Service | The date the service is rendered. |
| CPT | The general procedure code that was entered as the procedure billed on the case in charge entry. |
| ASA | The anesthesia procedure code that was entered as the procedure billed on the case in charge entry. |
| Billed | The amount billed for the procedure. |
| Expected | The amount of reimbursement expected from the payer or plan for the services rendered. This amount is calculated by the applicable expected fee schedule. |
| Control Number | The control number assigned to the insurance payment. |
| Allowed | The amount the payer will reimburse for the procedure. |
| Disallowed | The amount the payer will not reimburse for the procedure. |
| Payment | The amount of the payment. |
| Deductible | The specified amount of money that the insured must pay before an insurance company will pay a claim |
| Copay | A payment made by a beneficiary in addition to that made by an insurer. |
| Contractual Writeoffs | The calculated amount to be written off due to the contractual agreement between the practice and the primary payer. Contractual write-offs pertain only to the primary payer on the claim. The contractual write-off amount is the difference of the billed amount and the allow amount (Billed – Allow = Cont WO). |
| Withhold | The amount being withheld by the payer on the claim, as indicated on the EOB. Withholding is primarily associated with managed care, such as HMO plans. |
| Adjustments Negative | The sum of negative adjustments made against the payment. |
| Adjustments Positive | The sum of positive adjustments made against the payment. |
| Suspense | The amount of the Suspense balance received from guarantor or insurance payments. |
| Misc Income | The amount of the Misc Income balance received from guarantor or insurance payments. |
| Balance | The amount of the current balance on the procedure. |
Available Report Filters
Option | Type | Required | Description |
|---|---|---|---|
| Payment Batch ID | Free Text | No | The identification number associated with the payment batch to search and view in the report. |
| Report Folder | Drop Down | Yes | Designates where to place or save the output from the executed report. |