Overview
Purpose
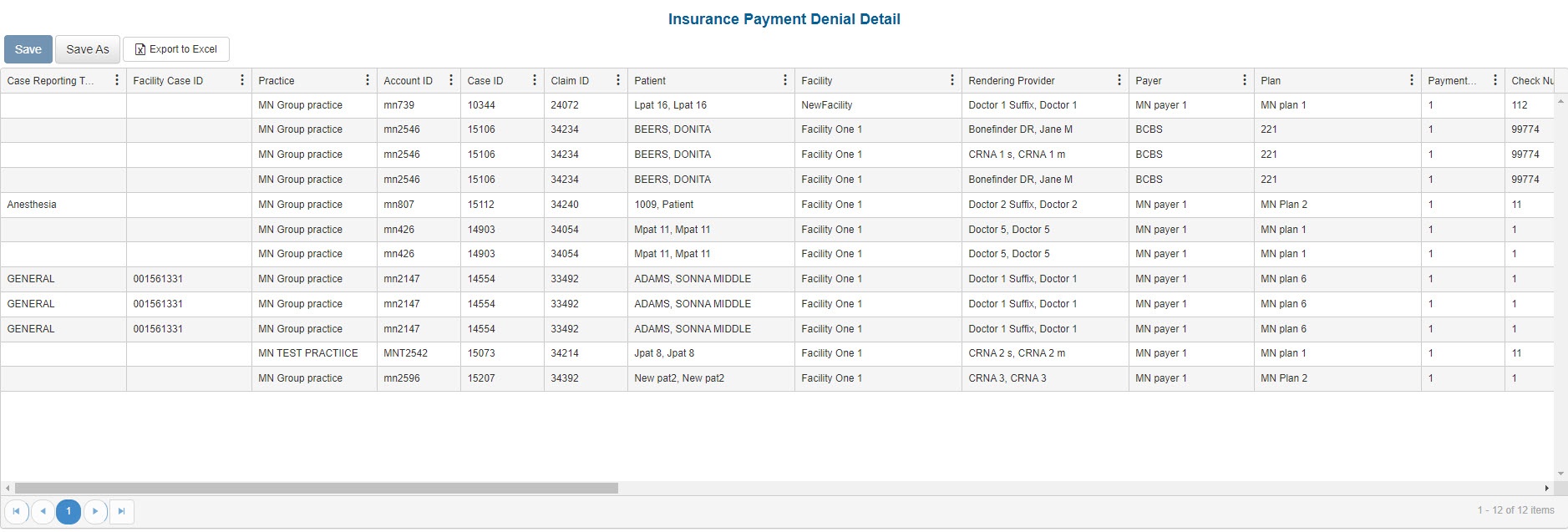
This report analyzes insurance denial details for a specified accounting or posted period.
Category
Financial
Type
Detail
Mode
Accounting / Posted
Output Options
CSV or Excel
Sample Reports
(Click an image to enlarge)
Portal
Back Office
Field Definitions
Field | Description |
|---|---|
| Case Reporting Type | The list of categories that can be associated to a case for reporting purposes, for example, Cardio (for treatments associated with the heart and lungs). |
| Facility Case ID | The identification number assigned to the case by the facility, for example, the hospital medical record. |
| Practice | The practice for which the charge is being billed. |
| Account ID | The account number of the guarantor account. Displays as Account Prefix + Account ID. |
| Case ID | The unique identification number assigned to the case. |
| Claim ID | The identification number issued to the claim when it was generated. |
| Patient | The name of the patient on the case. |
| Facility | The name of the facility where services were rendered. |
| Rendering Provider | The name of the provider (last name, first name) who performed the procedure on the case. |
| Payer | The primary insurance payer on the case with financial responsibility for the outstanding debt. |
| Plan | The primary insurance plan on the case to which charges were billed. |
| Payment Rank | The rank of the payer when there is one or more payers on the case. By default, this option is set to the primary payer. If the case has multiple payers, you can specify the rank of the payer to which a payment is being applied. |
| Check Number | The check number of the check. |
| Check Date | The date the check was written. |
| DOS | The date of service the procedure was performed. |
| CPT | The general procedure code of the service that was performed. |
| ASA | The anesthesia procedure code of the service that was performed. |
| Modifier 1 | The primary modifier entered on the procedure. |
| Modifier 2 | The second modifier entered on the procedure. |
| Billed | The billed amount of the procedure to which the denial was applied. |
| Balance | The current balance of the procedure to which the denial was applied. |
| Denial Group | The group to which the denial code on the claim is associated. |
| Denial Code | The unique identification for the denial reason for the claim. |
| Description | The explanation or reason for denying the claim. |
| Denied Amount | The amount from the claim that was denied by the insurance company. |
| Payment | The amount of payment received after receiving a denial. |
| Posted Date | The date the transaction was posted to the guarantor account. |
| Created Date | The date the denial payment distribution was created. |
| Pseudo Code | Codes used for user-created procedure codes. |
| Case Status | The status of the case. Options include: Unsubmitted, Submitted, On Hold, Reversed. |
| Claim Frequency | Classifies the claim as: Original, Corrected Replacement, Void. |
| Claim Submitted Date | The date the claim was submitted. |
Available Report Filters
Option | Type | Required | Description |
|---|---|---|---|
| Date Mode | Drop Down | Yes | Determines how the results are grouped and ordered:
|
| Date | Drop Down | Yes | Filters transactions displayed by the selected time period. Options include: Custom Date Range, Last # of Days, Today, Previous Day, Current Month, Previous Month, Current Year, and Previous Year. By default, this filter is set to Current Month. If Custom Date Range is selected, the From and To fields are enabled to enter specific dates to run the query on. If Last # of Days is selected, the Last # of Days field is enabled to enter a specific number of days to run the query on. |
| Practices | List Selection | No | Filters by all practices or by one or more practices. By default, this filter is set to All. Only active practices are returned in the search results. |
| Facilities | List Selection | No | Filters by all facilities or by one or more facilities. By default, this filter is set to All. |
| Providers | List Selection | No | Filters by all providers or by one or more providers. By default, this filter is set to All. |
| Payers | List Selection | No | Filters by payer to which the claims were submitted. By default, this filter is set to All. |
| Plans | List Selection | No | Filters by plan to which claims were submitted. By default, this filter is set to All. |
| Reason Code | List Selection | No | Filters transactions displayed by the selected payment denial reason code. |
| Report Folder | Drop Down | Yes | Designates where to place or save the output from the executed report. |
| Denial Code Group | List Selection | No | Filters transactions displayed by the selected payment denial reason code group. |