Overview
Purpose
This report summarizes posted charges and related financial activity for specified dates of service.
Category
Management
Type
Detail
Mode
Date of Service
Output Options
CSV or Excel
Sample Reports
(Click an image to enlarge)
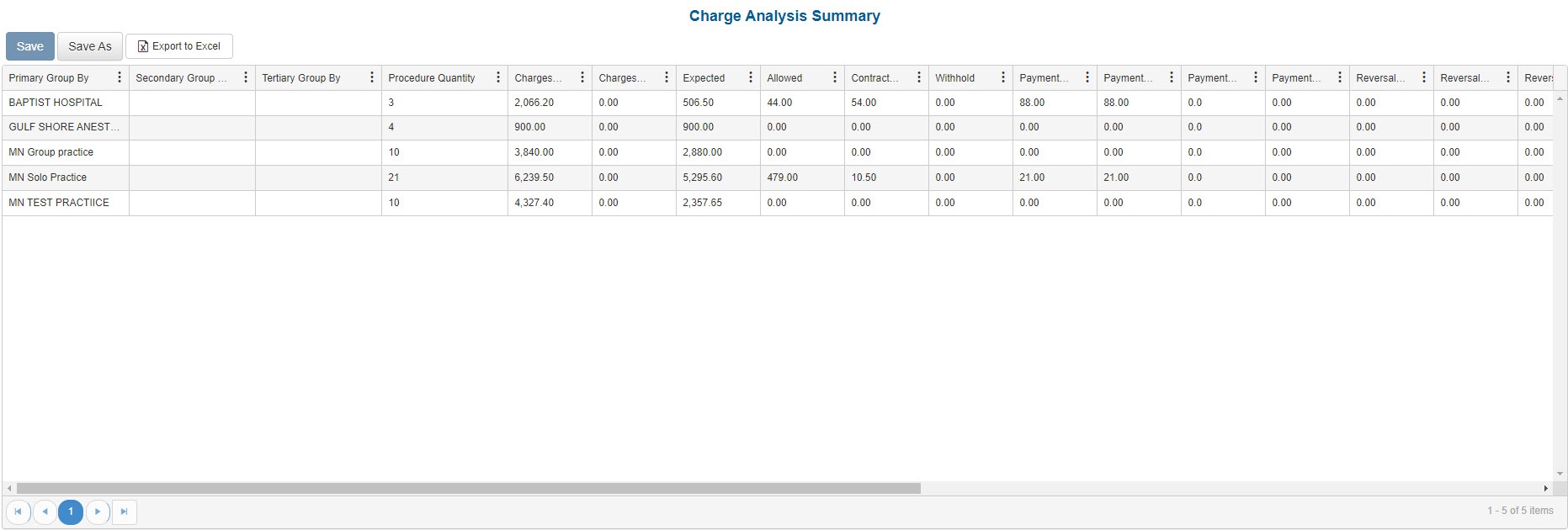
Portal
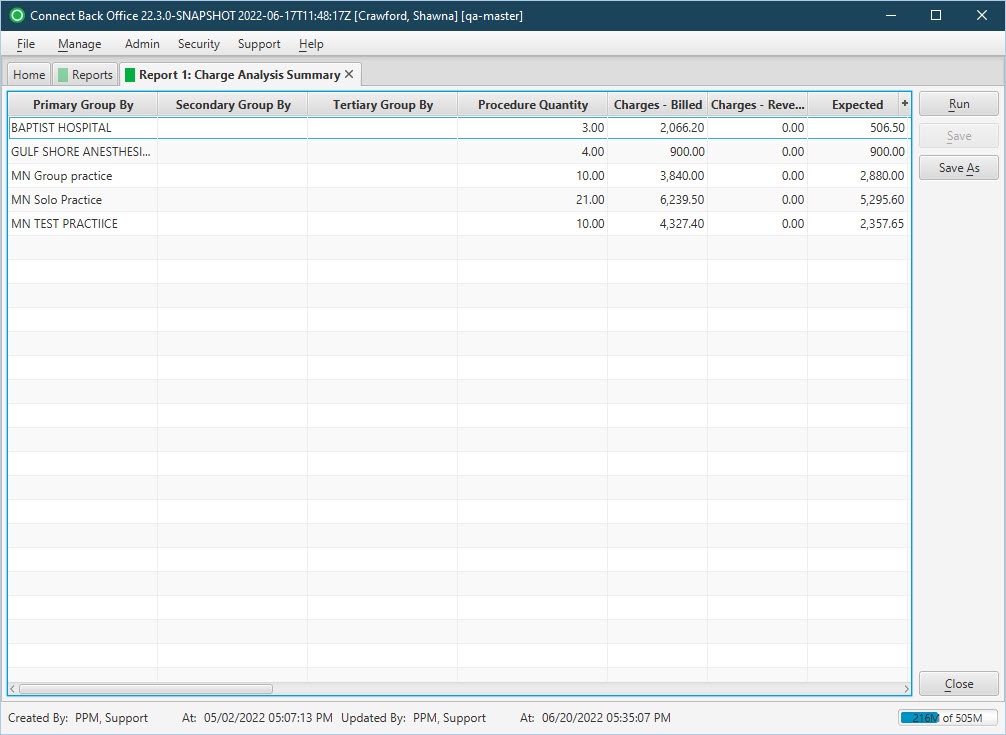
Back Office
Field Definitions
Field | Description |
|---|---|
| Primary / Secondary / Tertiary Group By | Displays the value for the selected Primary Group By, Secondary Group By, and Tertiary Group By filters. Options include: Practice, Facility, Rendering Provider, Payer, Plan, Case Reporting Type, Date of Service, Procedure Category, Procedure Code. |
| Procedure Quantity | The quantity of the procedure. |
| Charges - Billed | The amount billed for total charges for each service fee. |
| Charges - Reversed | All charges (SVCFE) that were reversed. |
| Expected | The amount expected for receipt from the payer for the service fee. |
| Allowed | The amount the payer will reimburse for the procedure. |
| Contractual Writeoff | The disallowed amount entered on the payment, which is taken as a negative adjustment. |
| Withhold | All withhold adjustments (additional payer adjustment) applied to the service line in payment entry. The amount held by the insurance company and applied as a credit to the SVCFE line item. |
| Payments - All | The amount distributed on a particular line item. |
| Payments - Insurance | The total amount of insurance payments received on a case. |
| Payments - Guarantor | The sum of payments applied on the guarantor account. |
| Payments - Suspense | The sum of payments applied on Suspense. |
| Reversals - All | The sum of all payment reversals. |
| Reversals - Insurance | The sum of payment reversals performed on insurance payments. |
| Reversals - Guarantor | The sum of payment reversals performed on guarantor payments. |
| Reversals - Suspense | The sum of payment reversals performed on suspense distributions. |
| Refunds | The total amount of refunds, or payments reversed, and posted from the account for the specified date range. |
| Adjustments - Negative | The sum of negative adjustments and reversals of negative adjustments performed on the service fee line. |
| Adjustments - Positive | The sum of positive adjustments and reversals of positive adjustments performed on the service fee line. |
| External Collections | The amount sent to external collections. |
| Balance | The current balance of the claim. |
| Base Units | The number of base units for each procedure on the case. |
| Time Units | The number of time units for each procedure on the case. |
| Physical Status Units | The number of physical units for each procedure on the case. |
| Total Units | The sum of base, time, and physical units billed. |
| Work RVU | The total work Relative Value Units on a procedure configured in the fee schedule. |
| Cases Count | The total number of cases as per the groupings. |
Available Report Filters
Option | Type | Required | Description |
|---|---|---|---|
| Date Mode | Drop Down | No | Determines how the results are grouped and ordered:
|
Date | Drop Down | Yes | Filters charges displayed by the selected time period. Options include: Custom Date Range, Last # of Days, Today, Previous Day, Current Month, Previous Month, Current Year, and Previous Year. If Custom Date Range is selected, the From and To fields are enabled to enter specific dates to run the query on. If Last # of Days is selected, the Last # of Days field is enabled to enter a specific number of days to run the query on. The maximum timespan for the report is 31 days. |
| Practices | List Selection | No | Filters by all practices or one or more practices for which charges were billed. By default, this filter is set to All. Only active practices are returned in the search results. |
| Providers | List Selection | No | Filters by all providers or by one or more providers. By default, this filter is set to All. |
| Provider Group | List Selection | No | Filters by one or more pre-designated groups of specific providers. By default, this filter is set to All. |
| Referring Providers | List Selection | No | Filters by all referring providers or by one or more referring providers. By default, this filter is set to All. |
| Facilities | List Selection | No | Filters by all facilities or by one or more facilities where services were rendered. By default, this filter is set to All. |
| Payers | List Selection | No | Filters by payer to which the claims were submitted. By default, this filter is set to All. |
| Plans | List Selection | No | Filters by plan to which claims were submitted. By default, this filter is set to All. |
| Financial Class | List Selection | No | Filters by all financial classes or by one or more financial classes. |
| Case Reporting Types | List Selection | No | Filters by case reporting types. By default, this filter is set to All. |
| Procedure Categories | List Selection | No | Filters by system and custom procedure categories. System-defined procedure categories are identified as (System), for example, Anesthesia (System). User-defined procedure categories are identified as (Custom), for example, Pain Management (Custom). By default, this filter is set to All. |
| Types of Service | List Selection | No | Filters by all types of service or by one or more types of service. By default, this filter is set to All. |
| Place of Service | List Selection | No | Filters by all places of service or by one or more places of service. By default, this filter is set to All. |
| CPT From/To | Text Entry | No | Filters by all CPT Codes in the entered range. |
| ASA From/To | Text Entry | No | Filters by all ASA Codes in the entered range. |
| Include Zero Balances | Checkbox | No | Filters by account balances, including those with zero balances. This filter does not include reversed service lines from rebill option 1. |
| Include Reversed Cases | Checkbox | No | Filters by cases, including reversed cases. The filter is unchecked by default and will not include reversed cases in search results unless checked. |
| Primary / Secondary / Tertiary Group By | Drop Down | Yes | These groups allow for arbitrary selection of up to three variables.
Options include: None, Practice, Facility, Rendering Provider, Payer, Plan, Case Reporting Type, Date of Service, Procedure Category, Procedure Code. |
| Report Folder | Drop Down | Yes | Designates where to place or save the output from the executed report. |