Overview
Purpose
This report analyzes posted case procedures for an accounting period or specified dates of service.
Category
Management
Type
Detail
Mode
Date of Service / Accounted / Posted
Output Options
CSV or Excel
Sample Reports
(Click an image to enlarge)
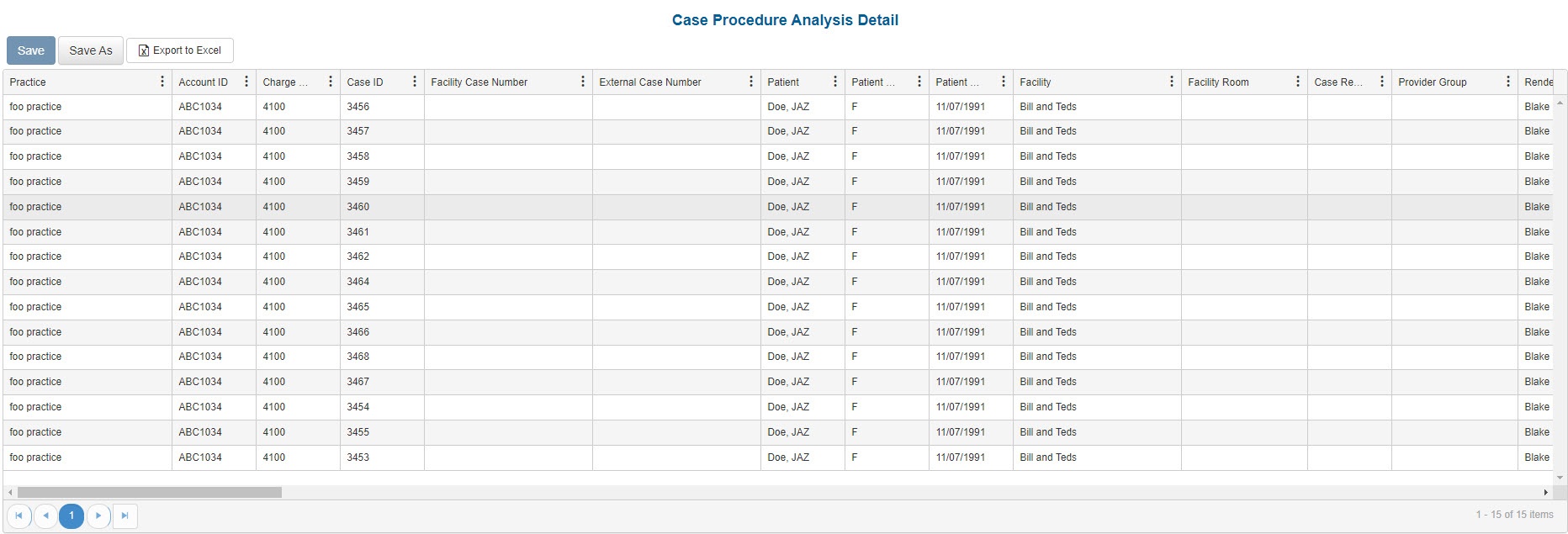
Portal
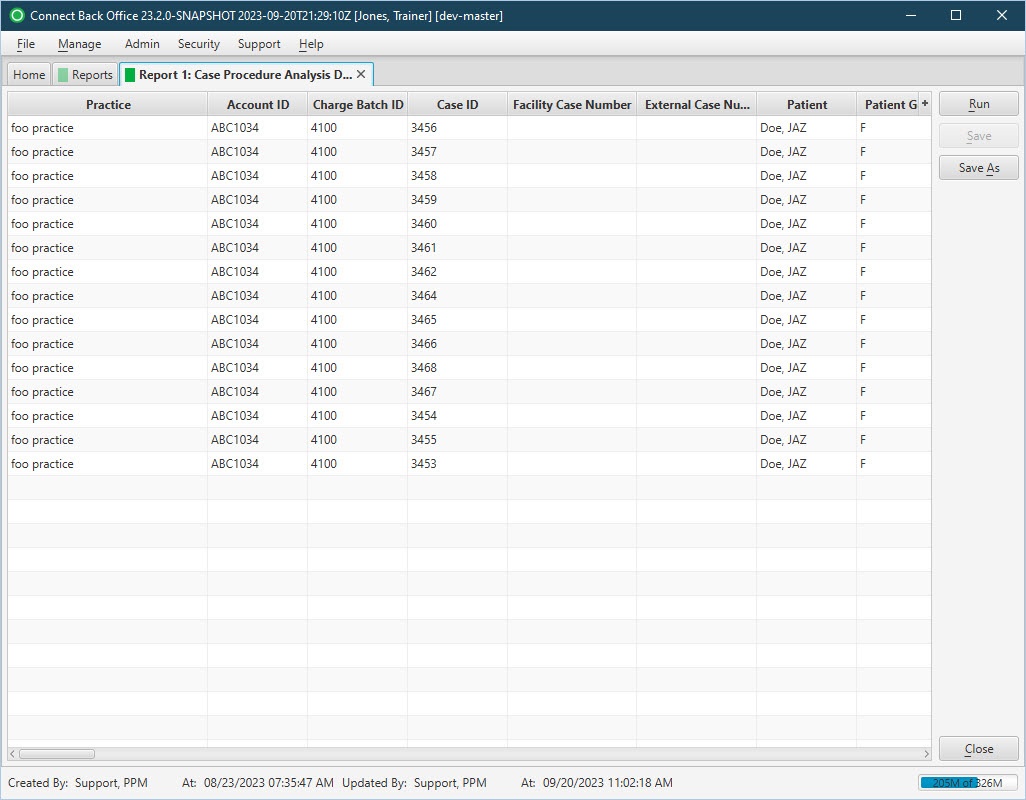
Back Office
Field Definitions
Field | Description |
|---|---|
| Practice | The practice for which the charge is being billed. |
| Account ID | The account number of the guarantor account. Displays as Account Prefix + Account ID. |
| Charge Batch ID | The unique number assigned to the charge batch. |
| Case ID | The unique number assigned to the case. |
| Facility Case Number | The case number issued by the facility, i.e., Medical Record Number. |
| External Case Number | An identification number for the case issued by a facility or payer. |
| Patient | The name of the patient. |
| Patient Gender | The gender of the patient. |
| Patient DOB | The date of birth of the patient. |
| Facility | The name of the facility where services were rendered. |
| Facility Room | The room number used at the facility, if provided. |
| Case Reporting Type | The unique code assigned to the case for identifying the case for reporting purposes. |
| Provider Group | The provider group assigned to the case for reporting purposes. |
| Rendering Provider | The name of the provider(s) who got credit for the case. This name, or names, can be affected by the Team Billing option selected for the relevant plan, e.g., Bill Physician Only, Bill Physician and CRNA on the same claim. |
| Rendering Provider Type | The classification of the type of rendering provider associated with the procedure on the charge. |
| Rendering Provider NPI | The national provider identification number issued to the rendering provider. |
| Referring Provider | The name of the physician who referred the patient. |
| Referring Provider Type | The specialty of the referring provider, based on the referring provider's specialty ID. |
| Referring Provider NPI | The national provider identification number issued to the referring provider. |
| Primary Payer | The primary insurance payer on the case with financial responsibility for the outstanding debt. |
| Primary Plan | The primary insurance plan on the case to which charges were billed. |
| Pre-Auth Number | The authorization number issued by the payer for authorization of the treatment or surgery. |
| Referral Number | The number issued by the primary or referring physician for a specific treatment or treatment series. Payment for services rendered may rely on whether a referral number is associated with a case. |
| Secondary Payer | The secondary payer on file for claims submission. |
| Date of Service - Case | The default date of service used for the case. |
| Date of Service - Procedure | The date of service for procedures. |
| Start Time | The time the anesthesia procedure began. |
| Stop Time | The time the anesthesia procedure ended. |
| Procedure Minutes | The total number of minutes for the associated procedure, anesthesia only. |
| Base Units | The number of base units for each procedure on the case. |
| Time Units | The number of time units for each procedure on the case. |
| Physical Status Units | The number of physical units for each procedure on the case |
| Total Units | The sum of base, time, and physical units billed. |
| Work RVU | The work relative value unit entered on the General procedure in the billing fee schedule to which the payer or plan is associated and to which the claim was billed. |
| Anesthesia Method | The method in which the anesthesia was administered to the patient. |
| Physical Status Level | The physical status of the patient, as indicated in charge entry. |
| Place of Service | The place where services are rendered. |
| Type of Service | The type of procedure: Anesthesia or General. |
| CPT | The general procedure code that was entered as the procedure billed on the case in charge entry. |
| CPT Short Description | A short description of the assigned CPT code. |
| ASA | The anesthesia procedure code that was entered as the procedure billed on the case in charge entry. |
| ASA Short Description | A short description of the assigned ASA code. |
| Modifier 1-4 | The primary (1st) througgh 4th modifiers entered on the procedure of the case. |
| Diagnosis 1-4 | The primary (1st) through 6th diagnosis entered on the case. |
| Procedure Quantity | The quantity of the procedure. |
| Billed | The amount billed for the procedure. |
| Expected | The amount expected for receipt from the payer for the service fee. |
| Balance | The current balance of the procedure line. |
| Accounting Date | The date within the accounting period when the charge was posted. The accounting date is stored at the practice configuration in Connect Back Office. |
| Charge Received Date | The date recorded on the case for when the charge was received. |
| Submitted Date | The date the case was submitted. |
| Submitted By | The name of the user that submitted the case. |
| Custom Fields | Any Charge Entry custom fields will display as columns at the end of the report. |
Available Report Filters
Results can be returned for one or more of the filter criteria (e.g., multiple practices).
Option | Type | Required | Description |
|---|---|---|---|
| Date Mode | Drop Down | Yes | Determines how the results are grouped and ordered:
If the report is run in Posted Date mode, it will not include cases that have not yet been submitted. |
| Date | Drop Down | Yes | Filters charges displayed by the selected time period. Options include: Custom Date Range, Last # of Days, Today, Previous Day, Current Month, Previous Month, Current Year, and Previous Year. If Custom Date Range is selected, the From and To fields are enabled to enter specific dates to run the query on. If Last # of Days is selected, the Last # of Days field is enabled to enter a specific number of days to run the query on. |
| Practices | List Selection | No | Filters by all practices, or one or more practices, for which charged were billed. By default, this filter is set to All. Only active practices are returned in the search results. |
| Providers | List Selection | No | Filters by all providers or by one or more providers. By default, this filter is set to All. |
| Provider Groups | List Selection | No | Filters by one or more pre-designated groups of specific providers. By default, this filter is set to All. |
| Referring Providers | List Selection | No | Filters by all referring providers or by one or more referring providers. By default, this filter is set to All. |
| Facilities | List Selection | No | Filters by all facilities, or by one or more facilities. By default, this filter is set to All. |
| Payers | List Selection | No | Filters by payers set as primary on the case. By default, this filter is set to All. |
| Plans | List Selection | No | Filters by plans set as primary on the case. By default, this filter is set to All. |
| Financial Class | List Selection | No | Filters by all financial classes or by one or more financial classes. By default, this filter is set to All. |
| Case Reporting Types | List Selection | No | Filters by all case reporting types or by one or more case reporting types. By default, this filter is set to All. |
| Procedure Categories | List Selection | No | Filters by system and custom procedure categories.
By default, this filter is set to All. |
| Type of Service | List Selection | No | Filters by all types of service, or by one or more types of service. By default, this filter is set to All. |
| Place of Service | List Selection | No | Filters by all places of service, or by one or more places of service. By default, this filter is set to All. |
| CPT From/To | Text Entry | No | Filters by all CPT Codes in the entered range. |
| ASA From/To | Text Entry | No | Filters by all ASA Codes in the entered range. |
| Include Reversed Cases | Checkbox | No | Filters by cases, including reversed cases. The filter is unchecked by default and will not include reversed cases in search results unless checked. |
| Report Folder | Drop Down | Yes | Designates where to place or save the output from the executed report. |