Overview
Purpose
This report analyzes posted or unposted case information.
Category
Management
Type
Detail
Mode
Date of Service / Accounted / Posted / Created
Output Options
CSV or Excel
Sample Reports
(Click an image to enlarge)
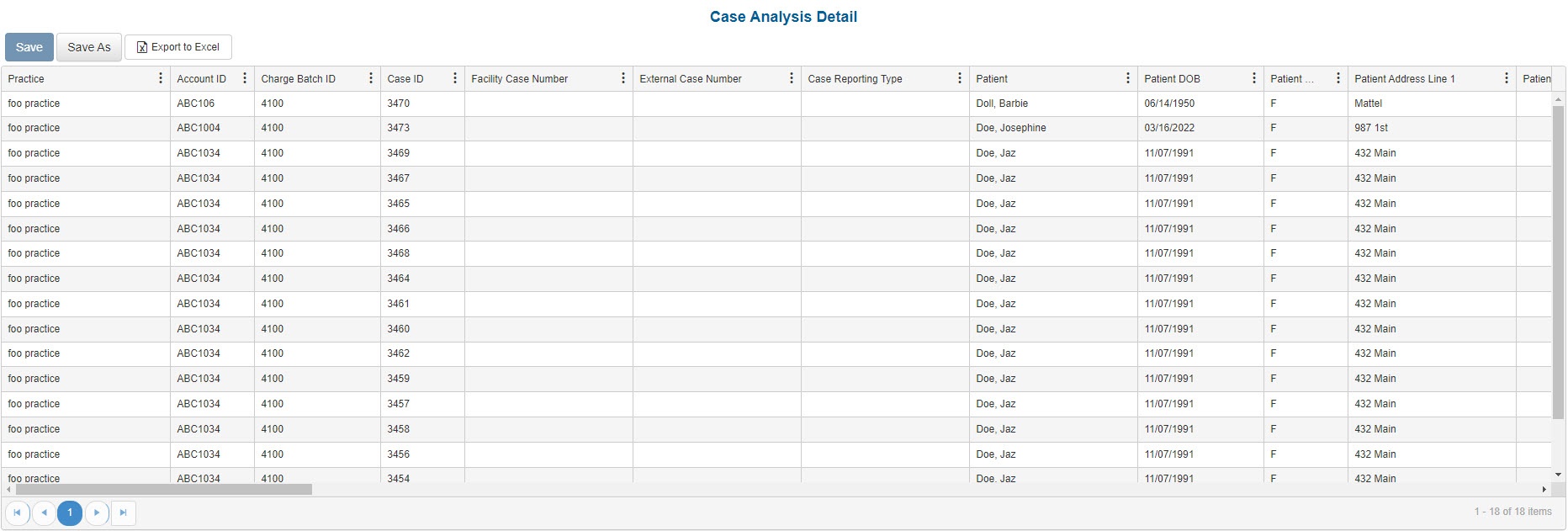
Portal
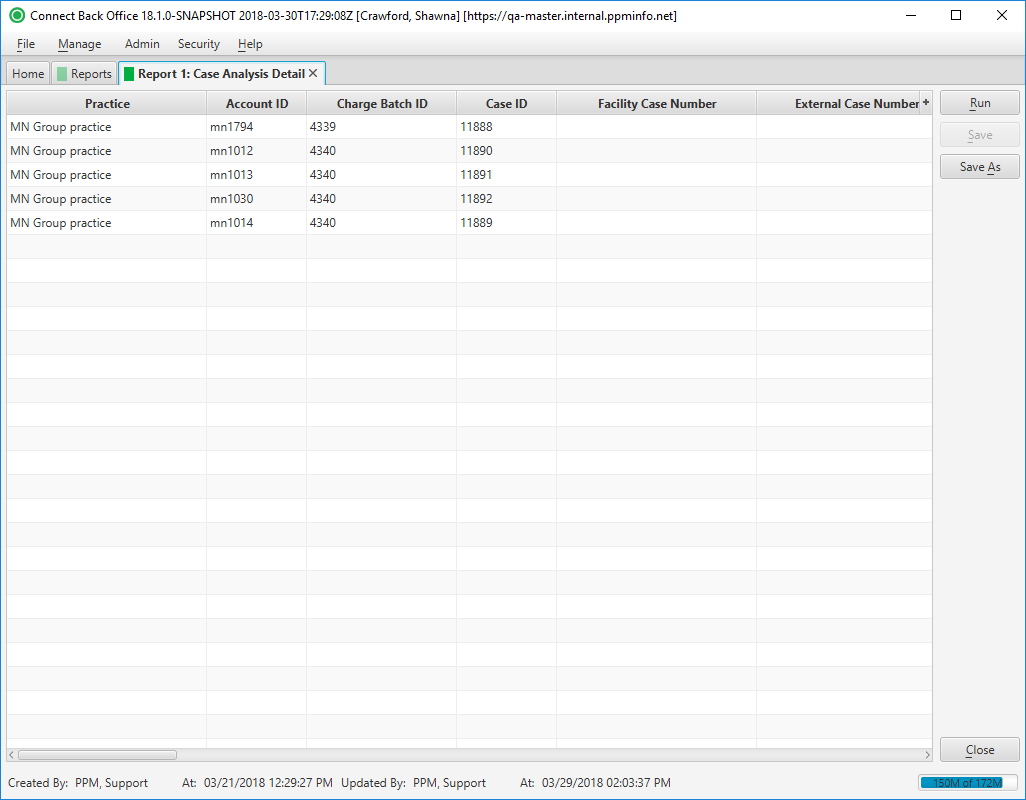
Back Office
Field Definitions
Field | Description |
|---|---|
| Practice | The practice for which the charge is being billed. |
| Account ID | The account number of the guarantor account. Displays as Account Prefix + Account ID. |
| Charge Batch ID | The unique number assigned to the charge batch. |
| Case ID | The unique number assigned to the case. |
| Facility Case Number | The case number issued by the facility, i.e., Medical Record Number. |
| External Case Number | An identification number for the case issued by a facility or payer. |
| Case Reporting Type | The unique code assigned to the case for identifying the case for reporting purposes. |
| Patient | The name of the patient. |
| Patient DOB | The date of birth of the patient. |
| Patient Gender | The gender of the patient. |
| Patient Address Line1 | The street address of the patient. |
| Patient Address Line 2 | The street address (line 2) of the patient. |
| Patient City | The city of the patient's address. |
| Patient State | The state of the patient's address. |
| Patient Zip Code | The zip code of the patient's address. |
| Guarantor | The financially responsible person or organization on the account. |
| Facility | The name of the facility where services were rendered. |
| Facility Room | The room the patient was assigned. |
| Place of Service | The place where services are rendered. Note: This list is maintained from the list of Place of Service codes by the Centers for Medicare & Medicaid Services (CMS). |
| Directing Provider | The name of the directing provider for the procedure (from the case). |
| Directed Provider | The name of the directed provider for the procedure (from the case). |
| Non-Anesthesia Provider | The provider for non-anesthesia services (from the case). |
| Referring Provider | The name of the physician who referred the patient. |
| Financial Class | Indicates in which grouping is the case’s plan. Financial class is used for reporting purposes. For example, you can set up either a managed care financial class or a more detailed breakdown delineating PPO and HMO classifications. |
| Primary Payer | The primary insurance payer on the case with financial responsibility for the outstanding debt. |
| Primary Plan | The primary insurance plan on the case to which charges were billed. |
| Primary Subscriber ID | The identification number of the primary insurance owner. |
| Primary Member ID | The unique number issued by the payer to identify the primary patient who participates in a group plan. |
| Primary Group ID | The unique number issued by the payer to the owner of the primary insurance policy. |
| Secondary Payer | The secondary payer on file for claims submission. |
| Secondary Plan | The secondary insurance plan on file for claims submission. |
| Secondary Subscriber ID | The identification number of the secondary insurance owner. |
| Secondary Member ID | The unique number issued by the payer to identify the secondary patient who participates in a group plan. |
| Secondary Group ID | The unique number issued by the payer to the owner of the secondary insurance policy. |
| Tertiary Payer | The tertiary payer on file for claims submission. |
| Tertiary Plan | The tertiary insurance plan on file for claims submission. |
| Tertiary Subscriber ID | The identification number of the tertiary insurance owner. |
| Tertiary Member ID | The unique number issued by the payer to identify the patient who participates in a tertiary group plan. |
| Tertiary Group ID | The unique number issued by the payer to the owner of the tertiary insurance policy. |
| Date of Service - Case | The date the service is rendered. |
| Start Time | The time the case started, e.g., 08:00. |
| Stop Time | The time the case ended, e.g., 09:00. |
| Addon Begin Time | The time the add-on procedure began, e.g., 08:30. |
| Concurrency Level | The level, or number of cases, the physician is working concurrently. |
| Anesthesia Method | Method used to administer anesthesia, e.g., General, Regional. |
| Physical Status Level | The physical status of the patient, as indicated in charge entry. |
| Case Type | The code indicating where a procedure was handled by a solo provider (S), two or more providers handing off (H), or a team of directing and directed providers (T). |
| Emergency | Indicates if the case is for an emergency procedure. |
| Diagnosis 1-6 | The primary (1st) through 6th diagnosis entered on the case. |
| Billed | The amount billed for the procedure. |
| Expected | The expected amount of payment from the responsible party for the amount billed, which is determined by the expected fee schedule configured at the practice configuration. |
| Payments - All | The sum of all payments and reversals associated to procedures on the case. This includes insurance payments, guarantor payments, payment reversals, rescinds, suspense payments, refunds, refund reversals, etc. |
| Adjustments | The sum of all adjustment types (CWO, Withhold, MADJN, MADJP, Adjusted CWO, External Collections, etc.) for all procedures on the case. |
| Balance | The outstanding balance on the account. |
| Collection % | The calculation for Payments / Billed. The percentage is rounded to the nearest tenth. |
| Case Status | The status of the case. Options include:
|
| Accounting Date | The date within the accounting period when the charge was posted. The accounting date is stored at the practice configuration in Connect Back Office. |
| Created Date | The date that the case was created. |
| Charge Received Date | The date recorded on the case for when the charge was received. |
| Posted Date | The date the transaction was posted to the guarantor account. |
Available Report Filters
Results can be returned for one or more of the filter criteria (e.g., multiple practices).
Option | Type | Required | Description |
|---|---|---|---|
| Date Mode | Drop Down | Yes | Determines how the results are grouped and ordered:
If the report is run in Posted Date mode, it will not include cases that have not yet been submitted. |
| Date | Drop Down | Yes | Filters transactions displayed by the selected time period. Options include: Custom Date Range, Last # of Days, Today, Previous Day, Current Month, Previous Month, Current Year, and Previous Year. If Custom Date Range is selected, the From and To fields are enabled to enter specific dates to run the query on. If Last # of Days is selected, the Last # of Days field is enabled to enter a specific number of days to run the query on. |
| Practices | List Selection | No | Filters by cases that include a reported outcome and a facility under the selected practice. |
| Providers | List Selection | No | Filters by all providers or by one or more providers. By default, this filter is set to All. |
| Provider Groups | List Selection | No | Filters by one or more pre-designated groups of specific providers. By default, this filter is set to All. |
| Referring Providers | List Selection | No | Filters by all referring providers or by one or more referring providers. By default, this filter is set to All. |
| Facilities | List Selection | No | Filters by cases that include a reported outcome and the facility/facilities selected. |
| Payers | List Selection | No | Filters by all payers or by one or more specific payers for which transactions were posted. By default, this filter is set to All. |
| Plans | List Selection | No | Filters by all plans or by one or more plans for which transactions were posted. By default, this filter is set to All. |
| Financial Class | List Selection | No | Filters by all financial classes or by one or more financial classes for which transactions were posted. By default, this filter is set to All. |
| Case Reporting Types | List Selection | No | Filters by all case reporting types or by one or more case reporting types. By default, this filter is set to All. |
| Place of Service | List Selection | No | Filters by all places of service or by one or more places of service. By default, this filter is set to All. |
| CPT From/To | Text Entry | No | Filters by all CPT Codes in the entered range. |
| ASA From/To | Text Entry | No | Filters by all ASA Codes in the entered range. |
| Room Numbers | List Selection | No | Filters by all rooms or by one or more room numbers. By default, this filter is set to All. |
| Status | Drop Down | No | Filters by all statuses or by one or more case statuses. By default, this filter is set to All. |
| Include Zero Balances | Checkbox | No | Filters by account balances, including those with zero balances. To exclude accounts with zero balances, clear this checkbox. |
| Include Reversed Cases | Checkbox | No | Include case data from cases that have been reversed. To exclude reversed cases, clear this checkbox. |
| Report Folder | Drop Down | Yes | Designates where to place or save the output from the executed report. |