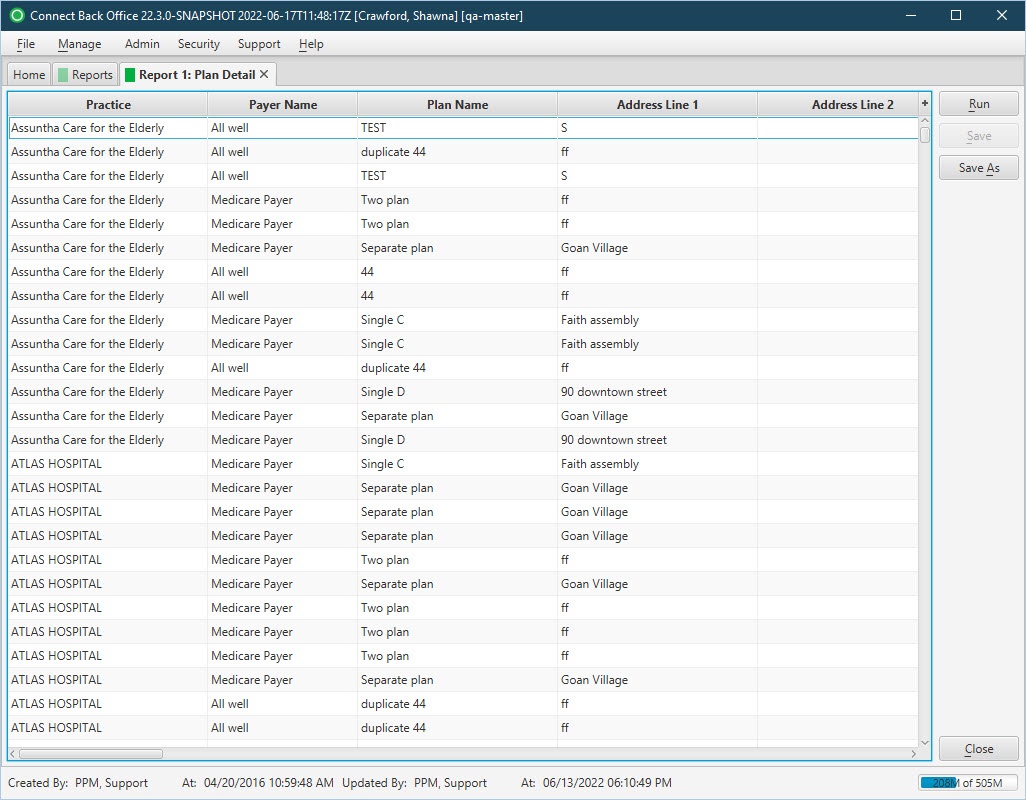
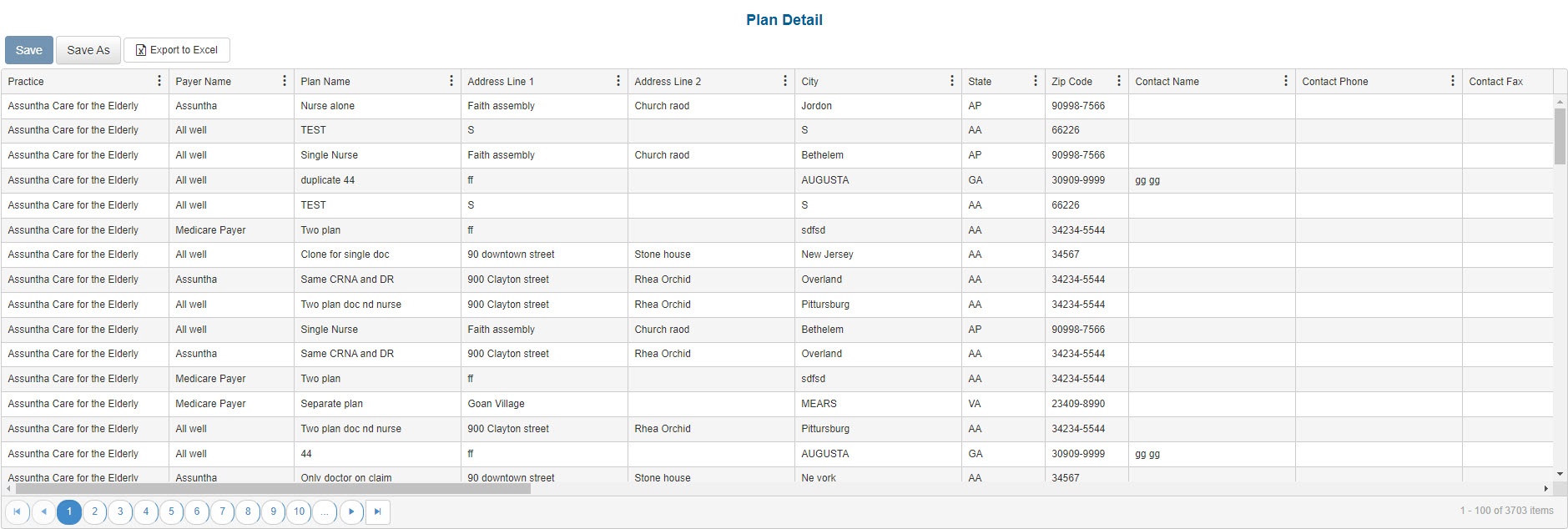
| Practice | The name of the practice. |
| Payer Name | The name of the parent payer to the plan. |
| Plan Name | The name of the plan. |
| Address Line 1 | The address line 1 of the street address of the plan. |
| Address Line 2 | The address line 2 of the street address of the plan. |
| City | The city of the plan. |
| State | The state of the plan. |
| Zip Code | The postal ZIP code of the plan. |
| Contact Name | The name of the primary contact for the plan. |
| Contact Phone | The 10-digit telephone number of the primary contact for the plan. |
| Contact Fax | The 10-digit facsimile number for the plan. |
| Contact Email | The electronic email address of the primary contact for the plan. |
| Website | The URL to the website for the plan. |
| Financial Class | Indicates the grouping the plan on the case is in. Financial class is used for reporting purposes. For example, you can set up either a managed care financial class or a more detailed break down delineating PPO and HMO classifications. |
| Clearinghouse | The name of the associated clearinghouse that distributes claims to the correct insurance payer. |
| Payer ID | The unique identification number of the plan for the clearinghouse. |
| Claim Type | The abbreviation that identifies the type of claims that will be generated for the plan, for example, Automobile Medical (AM), Commercial Insurance Company (CI), Disability and Health Maintenance Organization (HM). |
| Billing Provider Type | The provider type who is the billing provider when claims are generated. |
| Team Billing | The type that identifies whether claims include charges for a physician and a CRNA when involved on the same case that results in team billing. Claims can include charges for the physician only or the physician and CRNA, or the physician or CRNA. |
| Concurrency Scheme Name | The name of the concurrency scheme selected for the plan. |
| Extreme Age | Indicates whether the plan allows the extreme age modifier. |
| Emergency | Indicates whether the plan allows the emergency condition modifier. |
| Primary Claim Type | The primary claim format for the plan, e.g., Electronic, Drop to Paper, Self-Print. |
| Secondary Claim Type | The non-primary claim format for the plan, e.g., Electronic, Drop to Paper, Self-Print. |
| Paper Claim Form | The claim format used for paper submission of claims on the plan. |
| Effective Date | The effective date of the plan. |
| Expiration Date | The expiration date of the plan. |
| Network Status | Provides quick identification if the plan is in or out-of-network. |
| Contract Effective Date | The date the provider begins accepting the plan. |
| Inactive | A "Yes/No" flag to indicate if the plan is currently active. |
| Billed Fee Schedule | The name of billing fee schedule on the plan. |
| Expected Fee Schedule | The name of the expected fee schedule on the plan. |